Diagnosis
 Tachycardia consultation at Mayo Clinic
Tachycardia consultation at Mayo Clinic
A thorough physical exam, medical history and testing are required to diagnose tachycardia.
To diagnose tachycardia, a healthcare professional examines you and asks questions about your symptoms, health habits and medical history.
Tests
Electrocardiogram (ECG or EKG)

Electrocardiogram (ECG or EKG)
An electrocardiogram (ECG or EKG) is a simple test to determine how the heart is beating. Sensors, called electrodes, are placed on the chest to record the heart's electrical signals. The signals are shown as waves on an attached computer monitor or printer.
Holter monitor
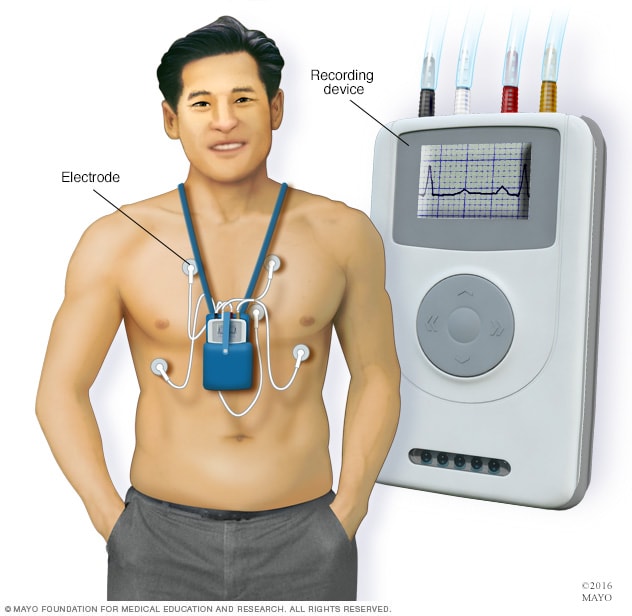
Holter monitor
A Holter monitor is a small, wearable device that continuously checks the heartbeat. It uses one or more sensors called electrodes and a recording device to measure the heart's activity. The device is typically worn for a day or more during daily activities.
Coronary angiogram
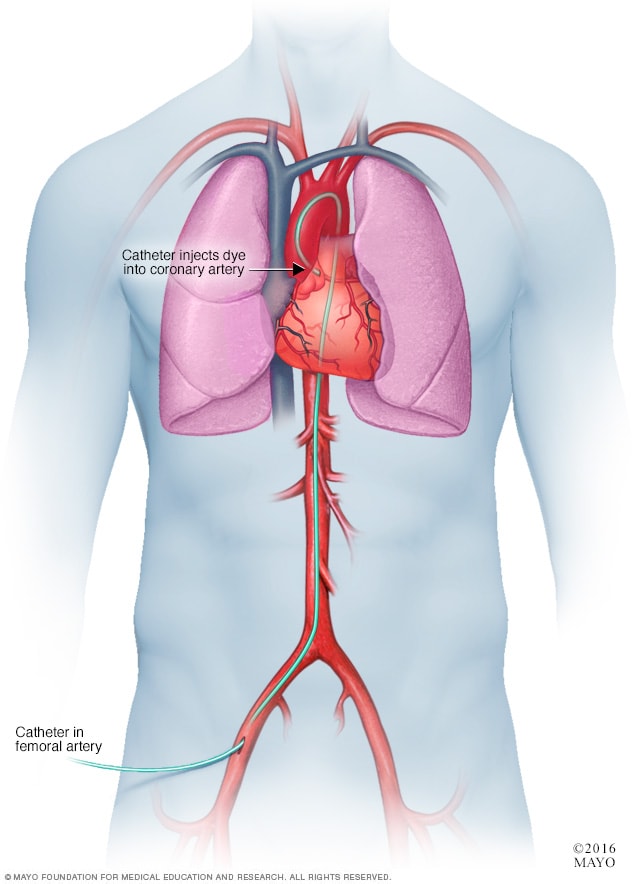
Coronary angiogram
In a coronary angiogram, a flexible tube called a catheter is inserted into an artery, usually in the groin, arm or neck. It's guided to the heart. A coronary angiogram can show blocked or narrowed blood vessels in the heart.
Tests may be done to confirm an unusually fast heartbeat and to look for the cause. Tests to diagnose tachycardia may include:
-
Electrocardiogram (ECG or EKG). This quick test checks the heartbeat. Sticky patches, called electrodes, are attached to the chest and sometimes to the arms or legs. An ECG shows how fast or how slow the heart is beating.
Some personal devices, such as smartwatches, can do ECGs. Ask your care team if this is an option for you.
- Holter monitor. This portable ECG device is worn for a day or more to record the heart's activity during daily activities. This test can detect irregular heartbeats that aren't found during a regular ECG exam.
- Event monitor. This device is like a Holter monitor, but it records only at certain times for a few minutes at a time. It's typically worn for about 30 days. You usually push a button when you feel symptoms. Some devices automatically record when an irregular heart rhythm is noticed.
- Echocardiogram. Sound waves are used to create images of the beating heart. This test can show how blood flows through the heart and heart valves.
- Chest X-ray. A chest X-ray shows the condition of the heart and lungs.
- MRI scan of the heart. Also called a cardiac MRI, this test uses magnetic fields and radio waves to create detailed images of the heart. It's most often done to find a cause of ventricular tachycardia or ventricular fibrillation.
- CT scan of the heart. Also called a cardiac CT, this test takes several X-ray images to provide a more detailed look of the heart. It may be done to find the cause of ventricular tachycardia.
- Coronary angiogram. A coronary angiogram is done to check for blocked or narrowed blood vessels in the heart. It uses a dye and special X-rays to show the inside of the coronary arteries. The test may be done to look at the heart's blood supply in people who have ventricular tachycardia or ventricular fibrillation.
-
Electrophysiological (EP) study. This test may be done to confirm a diagnosis of tachycardia. It can help find where in the heart the incorrect signaling occurs. An EP study is mostly used to diagnose some specific types of tachycardias and irregular heartbeats.
During this test, one or more flexible tubes are guided through a blood vessel, usually in the groin, to various areas in the heart. Sensors on the tips of the tubes record the heart's electrical signals.
- Stress tests. Exercise can trigger or worsen some types of tachycardia. Stress tests are done to see how exercise affects the heart. They often involve walking on a treadmill or pedaling a stationary bike while the heart is checked. If you can't exercise, you may be given medicine that increases the heart rate like exercise does. Sometimes an echocardiogram is done during a stress test.
- Tilt table test. This test may be done to learn if a fast heartbeat leads to fainting. The heart rate and rhythm and blood pressure are checked while you lie flat on a table. Then, under careful supervision, the table is tilted to a standing position. A member of your care team watches how your heart and the nervous system that controls it respond to the changes in position.
More Information
Treatment
The goals of tachycardia treatment are to slow a rapid heartbeat and to prevent future episodes of a fast heart rate.
If another health condition is causing tachycardia, treating the underlying problem may reduce or prevent episodes of a fast heartbeat.
Slowing a fast heart rate
A fast heart rate may correct itself. But sometimes medicine or other treatments are needed to slow down the heartbeat.
Ways to slow a fast heart rate include:
- Vagal maneuvers. Simple but specific actions such as coughing, bearing down as if passing stool or putting an ice pack on the face can help slow down the heart rate. Your healthcare team may ask you to do these specific actions during an episode of a fast heartbeat. The actions affect the vagus nerve. That nerve helps control the heartbeat.
- Medicines. If vagal maneuvers don't stop the fast heartbeat, medicine may be needed to correct the heart rhythm.
- Cardioversion. Paddles or patches on the chest are used to electrically shock the heart and reset the heart rhythm. Cardioversion is generally used when emergency care is needed or when vagal maneuvers and medicines don't work. It's also possible to do cardioversion with medicines.
Preventing future episodes of a fast heart rate
Tachycardia treatment involves taking steps to prevent the heart from beating too fast. This may involve medicines, implanted devices, or heart surgeries or procedures.
- Medicines. Medicines are often used to control the heart rate.
-
Catheter ablation. In this procedure, the doctor inserts thin, flexible tubes called catheters through a blood vessel, usually in the groin. Sensors on the tip of the catheters use heat or cold energy to create tiny scars in the heart. The scars block irregular electrical signals. This helps restore a typical heartbeat.
Catheter ablation doesn't require surgery to reach the heart, but it may be done at the same time as other heart surgeries.
- Pacemaker. A pacemaker is a small device that's surgically placed under the skin in the chest area. When the device senses an irregular heartbeat, it sends an electrical pulse that helps correct the heart's rhythm.
- Implantable cardioverter-defibrillator (ICD). This battery-powered device is placed under the skin near the collarbone. It continuously checks the heart rhythm. If the device detects an irregular heartbeat, it sends out low- or high-energy shocks to reset the heart's rhythm. A healthcare professional may recommend this device if you're at high risk of developing ventricular tachycardia or ventricular fibrillation.
- Maze procedure. A surgeon makes tiny cuts in the upper chambers of the heart to create a pattern of scar tissue. The pattern is called a maze. The heart's signals can't pass through scar tissue. So the maze can block stray electrical heart signals that cause some types of tachycardia.
- Surgery. Sometimes open-heart surgery is needed to destroy an extra electrical pathway causing tachycardia. Surgery is usually done only when other treatment options don't work or when surgery is needed to treat another heart condition.
 Tachycardia consultation at Mayo Clinic
Tachycardia consultation at Mayo Clinic
An implantable device, such as a pacemaker or implantable cardioverter-defibrillator (ICD), may be used to treat some types of tachycardia.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
If you have tachycardia or any type of heart disease, it's important to take steps to keep your heart healthy. Steps include lifestyle changes such as eating a heart-healthy diet, getting regular exercise, and not smoking or using tobacco. Your care team also may suggest that you limit or avoid caffeine.
Alternative medicine
Stress-relief techniques, such as meditation and yoga, might help slow the heartbeat. This can reduce tachycardia symptoms.
Coping and support
If you have a plan to manage an episode of a fast heartbeat, you may feel calmer and more in control when one occurs. Ask your care team:
- How to take your pulse and what heart rate is best for you.
- When and how to do treatments called vagal maneuvers, if appropriate.
- When to seek emergency care.
Preparing for your appointment
If you have tachycardia, you may see a doctor trained in heart conditions. This type of healthcare professional is called a cardiologist. You also might see a doctor trained in heart rhythm disorders, called an electrophysiologist.
There's often a lot to discuss at a health checkup. It's a good idea to be prepared for your appointment. Here's some information to help you get ready.
What you can do
Make a list ahead of time that you can share with your healthcare team. Your list should include:
- Any symptoms, including those that may seem unrelated to your heart.
- Important personal information, including any major stresses or recent life changes.
- All medicines that you take. Include vitamins, supplements and medicines bought with or without a prescription. Also include the dosages.
- Questions to ask your care team.
Basic questions to ask your healthcare professional include:
- What is the likely cause of my fast heart rate?
- What kinds of tests do I need?
- What's the most appropriate treatment?
- What are the risks of my heart condition?
- How do we check my heart?
- How often do I need follow-up appointments?
- How will other conditions I have or medicines I take affect my heart condition?
- Do I need to avoid or stop doing any activities?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend?
Don't hesitate to ask additional questions.
What to expect from your doctor
Your healthcare team is likely to ask you many questions. Being ready to answer them may save time to go over any details you want to spend more time on. Your care team may ask:
- When did the symptoms start?
- How often do you have episodes of a fast heartbeat?
- How long do they last?
- Does anything, such as exercise, stress or caffeine, make your symptoms worse?
- Does anyone in your family have heart disease or a history of irregular heart rhythms?
- Has anyone in your family had cardiac arrest or died suddenly?
- Do you smoke or have you ever smoked?
- How much alcohol or caffeine do you use, if any?
- What medicines do you take?
- Do you have any conditions that may affect your heart health? For example, are you being treated for high blood pressure or high cholesterol?
Dec. 15, 2023