Overview
Pulmonary atresia

Pulmonary atresia
In pulmonary atresia, the valve that lets blood flow from the heart to the lungs doesn't form as it should. Instead, some blood may enter the lungs through a temporary connection called the ductus arteriosus. The ductus arterious is between a baby's main artery, called the aorta, and the pulmonary artery. The right lower heart chamber, called the right ventricle, may be small in some babies with pulmonary atresia.
Pulmonary atresia (uh-TREE-zhuh) is a heart problem present at birth. That means it is a congenital heart defect. In this condition, the valve that helps move blood from the heart to the lungs doesn't form correctly. The valve is called the pulmonary valve.
Instead of a valve that opens and closes, a solid sheet of tissue forms. So, blood can't travel its usual path to get oxygen from the lungs. Instead, some blood travels to the lungs through other natural passages within the heart and its arteries.
A baby in the womb needs these other passages. But they usually close soon after birth.
Pulmonary atresia is a life-threatening condition that needs emergency treatment. Treatment includes surgery to repair the heart and medicines to help the heart work better.
Products & Services
Types
Symptoms
Symptoms of pulmonary atresia may be seen soon after birth. They can include:
- Blue or gray skin, lips or fingernails due to low oxygen levels. Depending on the skin color, these changes may be harder or easier to see.
- Fast breathing or shortness of breath.
- Tiring easily.
- Not feeding well.
When to see a doctor
Pulmonary atresia is most often found soon after birth. If your baby has symptoms of pulmonary atresia after you've left the hospital, get medical help right away.
Causes
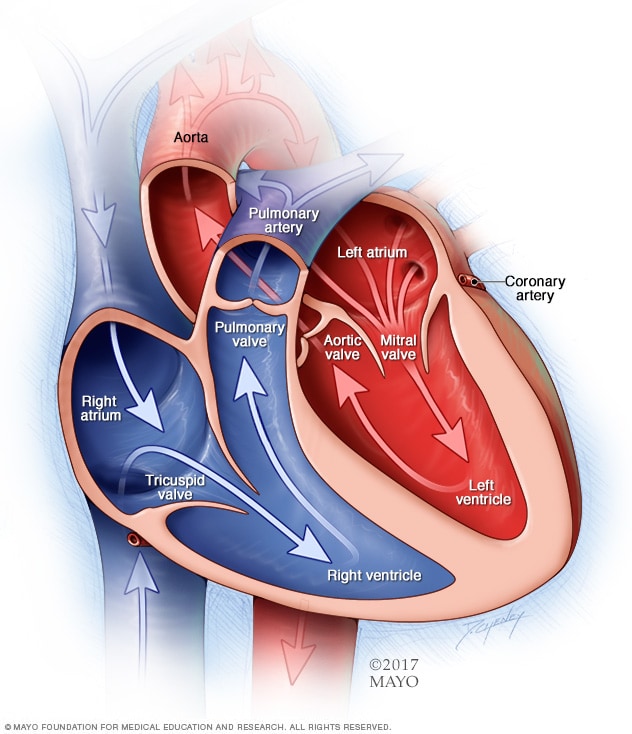
Chambers and valves of the heart
Chambers and valves of the heart
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves help keep blood flowing in the right direction.
The cause of pulmonary atresia is not clear. During the first six weeks of pregnancy, the baby's heart begins to form and starts beating. The major blood vessels that run to and from the heart also begin to develop during this critical time. It's at this point in a baby's development that a congenital heart defect such as pulmonary atresia may begin to develop.
To understand how pulmonary atresia occurs, it may be helpful to know how the heart works.
How the heart works
The typical heart is made of four chambers. There are two upper chambers, called atria, and two lower chambers, called ventricles.
The right side of the heart moves blood to the lungs. In the lungs, blood picks up oxygen and then returns it to the heart's left side. The left side of the heart then pumps the blood through the body's main artery, called the aorta. The blood goes to the rest of the body.
In pulmonary atresia, the pulmonary valve doesn't form as usual so it can't open. Blood can't flow from the right ventricle to the lungs.
Before birth, not having a pulmonary valve opening doesn't affect the baby's oxygen. That's because the baby gets oxygen from the tissue that connects the baby to the womb, called the placenta. The oxygen-rich blood from the placenta goes to the baby's right upper heart chamber.
The blood going into the right side of the baby's heart then passes through a hole between the top chambers of the baby's heart. The hole is called the foramen ovale. It lets oxygen-rich blood move to the rest of the baby's body through the aorta.
After birth, the lungs are needed for oxygen. In pulmonary atresia, without a working pulmonary valve, blood must find another way to reach the baby's lungs.
Blood from the right side of the heart can cross over the foramen ovale to the left heart. From there it can be pumped to the aorta. Newborn babies have a temporary opening called the ductus arteriosus between the aorta and the pulmonary artery. This opening lets some blood travel to the lungs. There the blood picks up oxygen to send to the rest of the baby's body.
The ductus arteriosus most often closes soon after birth. But medicines can keep it open.
Sometimes there's a second hole in the tissue between the main pumping chambers of the baby's heart. This hole is a ventricular septal defect (VSD).
The VSD lets blood flow from the right lower heart chamber to the left lower heart chamber. People with pulmonary atresia and a VSD often have other changes with the lungs and the arteries that bring blood to the lungs.
If there's no VSD, the right lower heart chamber gets little blood flow before birth. The chamber often doesn't form fully. This is a condition called pulmonary atresia with intact ventricular septum (PA/IVS).
Risk factors
Pulmonary atresia happens as the baby's heart is forming during pregnancy. Certain health conditions or illicit drug use during pregnancy may increase a baby's risk of pulmonary atresia or other congenital heart defects. Risk factors include:
- Obesity.
- Alcohol or tobacco use.
- Diabetes.
- Use of some types of medicines during pregnancy, such as certain acne and blood pressure medicines.
Some types of congenital heart defects occur in families. This means they are inherited. If you or someone in your family was born with a heart problem, including pulmonary atresia, ask your care team is genetic screening is right for you. Screening can help show the risk of certain congenital heart defects in future children.
Complications
Without treatment, pulmonary atresia most often leads to death. After surgery for pulmonary atresia, babies need regular health checkups throughout their lives to watch for complications.
Complications of pulmonary atresia may include:
- Bacterial infection of the inner lining of the heart and valves, called infectious endocarditis.
- Irregular heartbeats, called arrhythmias.
- Weakening of heart function.
Prevention
It might not be possible to prevent pulmonary atresia. But getting good prenatal care is important. Some things you can do before or during pregnancy might help lower your baby's risk of congenital heart defects. They include:
- Control other health conditions. If you have diabetes, keep your blood sugar in check. For other conditions that need medicines, talk to your healthcare professional about taking these medicines while pregnant.
- Don't smoke and don't be around others who smoke. If you smoke, quit. Smoking during pregnancy increases the risk of a congenital heart defect in the baby.
- Aim for a healthy weight. Obesity increases the risk of having a baby with a congenital heart defect.
- Get recommended vaccinations. Having rubella, also called German measles, during pregnancy can cause problems in a baby's heart development. A blood test done before pregnancy can determine if you're immune to rubella. A vaccine is available for those who aren't immune.