Overview
Claudication
Claudication
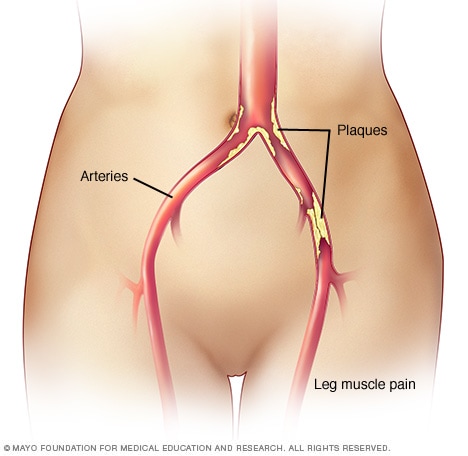
Claudication is pain in the legs or arms that occurs while walking or using the arms. The pain is caused by too little blood flow to the legs or arms. Claudication is usually a symptom of peripheral artery disease, in which the arteries that supply blood to the arms or legs, usually the legs, are narrowed. The narrowing is usually due to a buildup of fatty deposits, called plaque, on the artery walls.
Peripheral artery disease (PAD) is a common condition in which narrowed arteries reduce blood flow to the arms or legs.
This condition also may be called peripheral arterial disease.
In PAD, the legs or arms — usually the legs — don't get enough blood flow to keep up with demand. This may cause leg pain when walking, called claudication, and other symptoms.
Peripheral artery disease is usually a sign of a buildup of fatty deposits in the arteries, a condition called atherosclerosis.
Treatment for PAD includes exercising, eating healthy foods, and not smoking or using tobacco.
Products & Services
Symptoms
Peripheral artery disease (PAD) may not cause symptoms, or symptoms may be mild. PAD symptoms include:
- Leg pain when walking.
- Muscle pain or cramping in the arms or legs, often in the calf.
- Muscle pain in the arms or legs that begins with exercise and ends with rest.
- Painful cramping in one or both of the hips, thighs or calves after walking or climbing stairs or other activities.
- Pain when using the arms, such as aching and cramping when knitting or writing.
- Coldness in the lower leg or foot, especially when compared with the other side.
- Leg numbness or weakness.
- No pulse or a weak pulse in the legs or feet.
The muscle pain in peripheral artery disease may:
- Be mild to extreme.
- Wake you up from sleep.
- Make it hard to walk or exercise.
- Occur during rest or when lying down if the condition is severe.
Other symptoms of PAD may include:
- Shiny skin on the legs.
- Skin color changes on the legs.
- Slow-growing toenails.
- Sores on the toes, feet or legs that won't heal.
- Hair loss or slower hair growth on the legs.
- Erectile dysfunction.
When to see a doctor
Make an appointment for a health checkup if you have leg or arm pain or other symptoms of peripheral artery disease.
Causes
Development of atherosclerosis
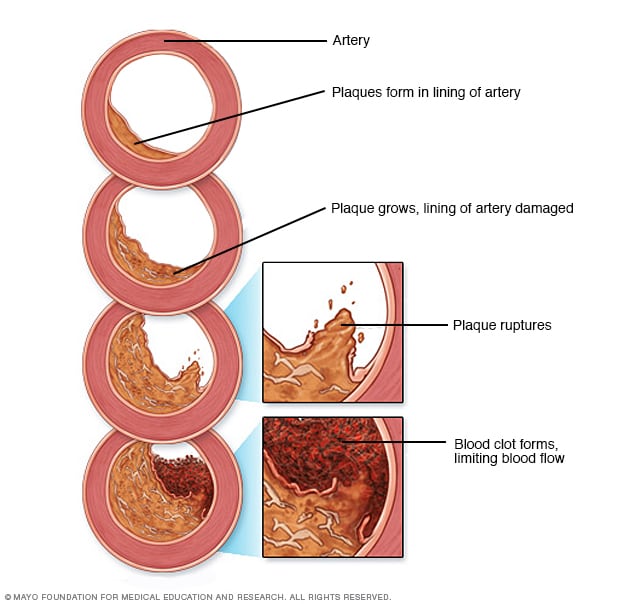
Development of atherosclerosis
If there's too much cholesterol in the blood, the cholesterol and other substances may form deposits called plaque. Plaque can cause an artery to become narrowed or blocked. If a plaque ruptures, a blood clot can form. Plaque and blood clots can reduce blood flow through an artery.
Peripheral artery disease (PAD) is often caused by a buildup of fats, cholesterol and other substances in and on the artery walls, a condition called atherosclerosis. The buildup is called plaque. Plaque can cause arteries to narrow, blocking blood flow. In PAD, plaque collects in the arteries of the arms or legs.
Less common causes of PAD include:
- Swelling and irritation of blood vessels.
- Injury to the arms or legs.
- Changes in the muscles or ligaments.
- Radiation exposure.
Risk factors
Risk factors for peripheral artery disease (PAD) include:
- A family history of peripheral artery disease, heart disease or stroke.
- Diabetes.
- High blood pressure.
- High cholesterol.
- Increasing age, especially after 65, or after 50 if you have risk factors for atherosclerosis.
- Obesity.
- Smoking.
Complications
Complications of peripheral artery disease (PAD) caused by atherosclerosis include:
- Critical limb ischemia. In this condition, an injury or infection causes tissue to die. Symptoms include open sores on the limbs that don't heal. Treatment may include amputation of the affected limb.
- Stroke and heart attack. Plaque buildup in the arteries also can affect the blood vessels in the heart and brain.
Prevention
The best way to prevent leg pain due to peripheral artery disease (PAD) is to have a healthy lifestyle. That means:
- Don't smoke.
- Eat foods that are low in sugar, trans fats and saturated fats.
- Get regular exercise — but check with your care team about what type and how much is best for you.
- Keep a healthy weight.
- Manage blood pressure, cholesterol and diabetes.
- Get good sleep.
- Control stress.
Aug. 09, 2024