Overview
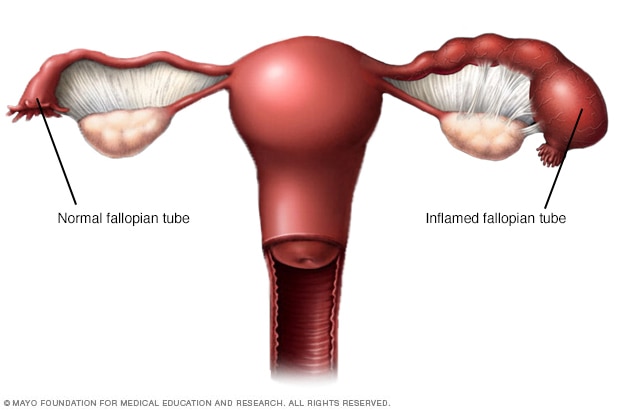
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs. It most often occurs when sexually transmitted bacteria spread from your vagina to your uterus, fallopian tubes or ovaries.
Pelvic inflammatory disease
Pelvic inflammatory disease (PID) is an infection of one or more of the upper reproductive organs, including the uterus, fallopian tubes and ovaries. Untreated can cause scar tissue and pockets of infected fluid (abscesses) to develop in the reproductive tract, which can cause permanent damage.
The signs and symptoms of pelvic inflammatory disease can be subtle or mild. Some women don't experience any signs or symptoms. As a result, you might not realize you have it until you have trouble getting pregnant or you develop chronic pelvic pain.
Symptoms
The signs and symptoms of pelvic inflammatory disease might be mild and difficult to recognize. Some women don't have any signs or symptoms. When signs and symptoms of pelvic inflammatory disease (PID) are present, they most often include:
- Pain — ranging from mild to severe — in your lower abdomen and pelvis
- Unusual or heavy vaginal discharge that may have an unpleasant odor
- Unusual bleeding from the vagina, especially during or after sex, or between periods
- Pain during sex
- Fever, sometimes with chills
- Painful, frequent or difficult urination
When to see a doctor
See your health care provider or seek urgent medical care if you experience:
- Severe pain low in your abdomen
- Nausea and vomiting, with an inability to keep anything down
- Fever, with a temperature higher than 101 F (38.3 C)
- Foul vaginal discharge
If you have signs and symptoms of PID that aren't severe, still see your provider as soon as possible. Vaginal discharge with an odor, painful urination or bleeding between periods can also be symptoms of a sexually transmitted infection (STI). If these signs and symptoms occur, stop having sex and see your provider soon. Prompt treatment of an sexually transmitted infection (STI) can help prevent PID.
Women’s health topics – straight to your inbox
Causes
Many types of bacteria can cause PID, but gonorrhea or chlamydia infections are the most common. These bacteria are usually acquired during unprotected sex.
Less commonly, bacteria can enter your reproductive tract anytime the normal barrier created by the cervix is disturbed. This can happen during menstruation and after childbirth, miscarriage or abortion. Rarely, bacteria can also enter the reproductive tract during the insertion of an intrauterine device (IUD) — a form of long-term birth control — or any medical procedure that involves inserting instruments into the uterus.
Risk factors
A number of factors might increase your risk of pelvic inflammatory disease, including:
- Being sexually active and younger than 25 years old
- Having multiple sexual partners
- Being in a sexual relationship with someone who has more than one sex partner
- Having sex without a condom
- Douching regularly, which upsets the balance of good versus harmful bacteria in the vagina and might mask symptoms
- Having a history of pelvic inflammatory disease or a sexually transmitted infection
There is a small increased risk of PID after the insertion of an intrauterine device (IUD). This risk is generally confined to the first three weeks after insertion.
Complications
Untreated pelvic inflammatory disease might cause scar tissue and pockets of infected fluid (abscesses) to develop in the reproductive tract. These can cause permanent damage to the reproductive organs.
Complications from this damage might include:
- Ectopic pregnancy. PID is a major cause of tubal (ectopic) pregnancy. An ectopic pregnancy can occur when untreated PID has caused scar tissue to develop in the fallopian tubes. The scar tissue prevents the fertilized egg from making its way through the fallopian tube to implant in the uterus. Instead, the egg implants in the fallopian tube. Ectopic pregnancies can cause massive, life-threatening bleeding and require emergency medical attention.
- Infertility. Damage to your reproductive organs may cause infertility — the inability to become pregnant. The more times you've had PID, the greater your risk of infertility. Delaying treatment for PID also dramatically increases your risk of infertility.
- Chronic pelvic pain. Pelvic inflammatory disease can cause pelvic pain that might last for months or years. Scarring in your fallopian tubes and other pelvic organs can cause pain during intercourse and ovulation.
- Tubo-ovarian abscess. PID might cause an abscess — a collection of pus — to form in your reproductive tract. Most commonly, abscesses affect the fallopian tubes and ovaries, but they can also develop in the uterus or in other pelvic organs. If an abscess is left untreated, you could develop a life-threatening infection.
Prevention
To reduce your risk of pelvic inflammatory disease:
- Practice safe sex. Use condoms every time you have sex, limit your number of partners and ask about a potential partner's sexual history.
- Talk to your health care provider about contraception. Many forms of contraception do not protect against the development of PID. Using barrier methods, such as a condom, helps to reduce your risk. Even if you take birth control pills, use a condom every time you have sex with a new partner to protect against STIs.
- Get tested. If you're at risk of an STI, make an appointment with your provider for testing. Set up a regular screening schedule with your provider if needed. Early treatment of an STI gives you the best chance of avoiding PID.
- Request that your partner be tested. If you have pelvic inflammatory disease or an STI, advise your partner to be tested and treated. This can prevent the spread of STIs and possible recurrence of PID.
- Don't douche. Douching upsets the balance of bacteria in your vagina.