Diagnosis
Pelvic exam
Pelvic exam
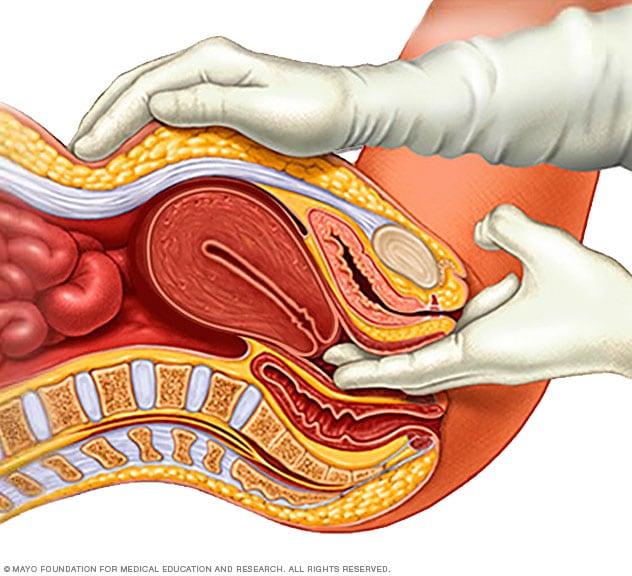
During a pelvic exam, a doctor inserts one or two gloved fingers inside the vagina. Pressing down on the abdomen at the same time, the doctor can check the uterus, ovaries and other organs.
Tests and procedures used to diagnose ovarian cancer include:
- Pelvic exam. During a pelvic exam, your doctor inserts gloved fingers into your vagina and simultaneously presses a hand on your abdomen in order to feel (palpate) your pelvic organs. The doctor also visually examines your external genitalia, vagina and cervix.
- Imaging tests. Tests, such as ultrasound or CT scans of your abdomen and pelvis, may help determine the size, shape and structure of your ovaries.
-
Blood tests. Blood tests might include organ function tests that can help determine your overall health.
Your doctor might also test your blood for tumor markers that indicate ovarian cancer. For example, a cancer antigen (CA) 125 test can detect a protein that's often found on the surface of ovarian cancer cells. These tests can't tell your doctor whether you have cancer, but they may provide clues about your diagnosis and prognosis.
- Surgery. Sometimes your doctor can't be certain of your diagnosis until you undergo surgery to remove an ovary and have it tested for signs of cancer.
- Genetic testing. Your doctor may recommend testing a sample of your blood to look for gene changes that increase the risk of ovarian cancer. Knowing you have an inherited change in your DNA helps your doctor make decisions about your treatment plan. You may wish to share the information with your blood relatives, such as your siblings and your children, since they also may have a risk of having those same gene changes.
Once it's confirmed that you have ovarian cancer, your doctor will use information from your tests and procedures to assign your cancer a stage. The stages of ovarian cancer range from 1 to 4, which are often indicated with Roman numerals I to IV. The lowest stage indicates that the cancer is confined to the ovaries. By stage 4, the cancer has spread to distant areas of the body.
More Information
Treatment
Treatment of ovarian cancer usually involves a combination of surgery and chemotherapy. Other treatments may be used in certain situations.
Surgery
Operations to remove ovarian cancer include:
- Surgery to remove one ovary. For early-stage cancer that hasn't spread beyond one ovary, surgery may involve removing the affected ovary and its fallopian tube. This procedure may preserve your ability to have children.
- Surgery to remove both ovaries. If cancer is present in both your ovaries, but there are no signs of additional cancer, your surgeon may remove both ovaries and both fallopian tubes. This procedure leaves your uterus intact, so you may still be able to become pregnant using your own frozen embryos or eggs or with eggs from a donor.
- Surgery to remove both ovaries and the uterus. If your cancer is more extensive or if you don't wish to preserve your ability to have children, your surgeon will remove the ovaries, the fallopian tubes, the uterus, nearby lymph nodes and a fold of fatty abdominal tissue (omentum).
- Surgery for advanced cancer. If your cancer is advanced, your doctor may recommend surgery to remove as much of the cancer as possible. Sometimes chemotherapy is given before or after surgery in this situation.
Chemotherapy
Chemotherapy is a drug treatment that uses chemicals to kill fast-growing cells in the body, including cancer cells. Chemotherapy drugs can be injected into a vein or taken by mouth.
Chemotherapy is often used after surgery to kill any cancer cells that might remain. It can also be used before surgery.
In certain situations, chemotherapy drugs may be heated and infused into the abdomen during surgery (hyperthermic intraperitoneal chemotherapy). The drugs are left in place for a certain amount of time before they're drained. Then the operation is completed.
Targeted therapy
Targeted drug treatments focus on specific weaknesses present within cancer cells. By attacking these weaknesses, targeted drug treatments can cause cancer cells to die.
If you're considering targeted therapy for ovarian cancer, your doctor may test your cancer cells to determine which targeted therapy is most likely to have an effect on your cancer.
Hormone therapy
Hormone therapy uses drugs to block the effects of the hormone estrogen on ovarian cancer cells. Some ovarian cancer cells use estrogen to help them grow, so blocking estrogen may help control the cancer.
Hormone therapy might be a treatment option for some types of slow-growing ovarian cancers. It may also be an option if the cancer comes back after initial treatments.
Immunotherapy
Immunotherapy uses the immune system to fight cancer. The body's disease-fighting immune system may not attack cancer cells because they produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process.
Immunotherapy might be an option for treating ovarian cancer in certain situations.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care. Palliative care can be used while undergoing other aggressive treatments, such as surgery and chemotherapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
Palliative care is provided by a team of doctors, nurses and other specially trained professionals. Palliative care teams aim to improve the quality of life for people with cancer and their families. This form of care is offered alongside curative or other treatments you may be receiving.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
A diagnosis of ovarian cancer can be overwhelming. In time you'll find ways to cope with your feelings, but in the meantime, you might find it helpful to:
- Find someone to talk with. You may feel comfortable discussing your feelings with a friend or family member, or you might prefer meeting with a formal support group. Support groups for the families of people with cancer also are available.
- Let people help. Cancer treatments can be exhausting. Let people know what would be most useful for you.
- Set reasonable goals. Having goals helps you feel in control and can give you a sense of purpose. But choose goals that you can reach.
- Take time for yourself. Eating well, relaxing and getting enough rest can help combat the stress and fatigue of cancer.
Preparing for your appointment
Start by making an appointment with your family doctor or gynecologist if you have any signs or symptoms that worry you.
If your primary care doctor suspects that you have ovarian cancer, you may be referred to a specialist in female reproductive cancers (gynecological oncologist). A gynecological oncologist is an obstetrician-gynecologist (OB-GYN) who has additional training in the diagnosis and treatment of ovarian cancer and other gynecological cancers.
What you can do
- Be aware of any pre-appointment restrictions, such as not eating solid food on the day before your appointment.
- Write down your symptoms, including any that may seem unrelated to the reason why you scheduled the appointment.
- Write down your key medical information, including other conditions.
- Write down key personal information, including any major changes or stressors in your life.
- Make a list of all your medications, vitamins or supplements.
- Ask a relative or friend to accompany you, to help you remember what the doctor says.
- Write down questions to ask your doctor.
Questions to ask your doctor
- What's the most likely cause of my symptoms?
- What kinds of tests do I need?
- What treatments are available, and what side effects can I expect?
- What is the prognosis?
- If I still want to have children, what options are available to me?
- I have other health conditions. How can I best manage them together?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask other questions that occur to you.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may make time to go over points you want to spend more time on. You may be asked:
- When did you first begin experiencing symptoms, and how severe are they?
- Have your symptoms been continuous or occasional?
- What, if anything, seems to improve or worsen your symptoms?
- Do you have any relatives with ovarian or breast cancer?
- Are there other cancers in your family history?
Jan. 10, 2025