Diagnosis
During the physical exam, your healthcare professional checks your affected joint for tenderness, swelling and flexibility.
Imaging tests
To get pictures of the affected joint, your healthcare professional might recommend:
- X-rays. Cartilage doesn't show up on X-ray images, but cartilage loss is revealed by a narrowing of the space between the bones in your joint. An X-ray also can show bone spurs around a joint.
- Magnetic resonance imaging (MRI). An MRI uses radio waves and a strong magnetic field to produce detailed images of bone and soft tissues, including cartilage. An MRI isn't commonly needed to diagnose osteoarthritis but can help provide more information in complex cases.
Lab tests
Analyzing blood or joint fluid can help confirm the diagnosis.
- Blood tests. Although there's no blood test for osteoarthritis, certain tests can help rule out other causes of joint pain, such as rheumatoid arthritis.
- Joint fluid analysis. A needle might be used to draw fluid from an affected joint. The fluid is then tested to determine whether your pain is caused by an inflammatory arthritis, such as rheumatoid arthritis or gout, or an infection rather than osteoarthritis.
Treatment
Osteoarthritis can't be reversed, but treatments can reduce pain and help you move better.
Medicines
Medicines that can help relieve osteoarthritis pain symptoms include:
- Acetaminophen. Acetaminophen (Tylenol, others) has been shown to help some people with osteoarthritis who have mild to moderate pain. Taking more than the recommended dose of acetaminophen can cause liver damage.
-
Nonsteroidal anti-inflammatory drugs (NSAIDs). Common pain relievers, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve), taken at the recommended doses, typically relieve osteoarthritis pain. Stronger NSAIDs are available by prescription.
NSAIDs can cause stomach upset, cardiovascular problems, bleeding problems, and liver and kidney damage. NSAIDs as gels, applied to the skin over the affected joint, have fewer side effects and may relieve pain just as well.
- Duloxetine (Cymbalta). Although typically used as an antidepressant, duloxetine also is approved to treat chronic pain, including osteoarthritis pain.
Therapy
- Physical therapy. A physical therapist can show you exercises to strengthen the muscles around your joint, increase your flexibility and reduce pain. Regular gentle exercise that you do on your own, such as swimming or walking, can be equally effective.
- Occupational therapy. An occupational therapist can help you find ways to do everyday tasks without putting extra stress on an already painful joint. For instance, a toothbrush with a large grip could make brushing your teeth easier if you have osteoarthritis in your hands. A bench in your shower could help relieve the pain of standing if you have knee osteoarthritis.
- Transcutaneous electrical nerve stimulation (TENS). This uses a low-voltage electrical current to relieve pain. It provides short-term relief for some people with knee and hip osteoarthritis.
Surgical and other procedures
If conservative treatments don't help, you might want to consider procedures such as:
- Cortisone injections. Injections of a corticosteroid into the joint might relieve pain for a few weeks. The number of cortisone injections you can receive each year is generally limited to three or four, because the medicine can worsen joint damage over time.
- Lubrication injections. Injections of hyaluronic acid might relieve pain by providing some cushioning in your knee, though some research suggests that these injections offer no more relief than a placebo. Hyaluronic acid is similar to a component typically found in joint fluid.
- Realigning bones. If osteoarthritis has damaged one side of your knee more than the other, an osteotomy might be helpful. In a knee osteotomy, a surgeon cuts across the bone either above or below the knee and removes or adds a wedge of bone. This shifts your body weight away from the worn-out part of your knee.
- Joint replacement. In joint replacement surgery, the surgeon removes the damaged joint surfaces and replaces them with plastic and metal parts. Surgical risks include infections and blood clots. Artificial joints can wear out or come loose and might need to be replaced.

Knee osteotomy
For some people, arthritis damages one side of the knee more than the other side. This can cause your knee to bow inward or outward. Removing or adding a wedge of bone in your shinbone or thighbone can help straighten this bowing and shift your weight to the undamaged part of your knee joint.

Artificial hip
Hip prostheses are designed to mimic the ball-and-socket action of your hip joint. During hip replacement surgery, your surgeon removes the diseased or damaged parts of your hip joint and inserts the artificial joint.
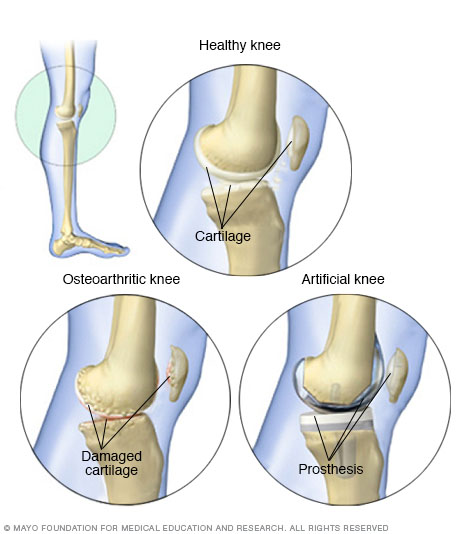
Knee comparisons
One of the most common reasons for knee replacement surgery is severe pain from joint damage caused by osteoarthritis. This condition can break down the slick cartilage that helps your knee joint move smoothly. An artificial knee joint has metal alloy caps for your thighbone and shinbone and high-density plastic to replace damaged cartilage.
From Mayo Clinic to your inbox
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Self care
Learn all you can about your condition and how to manage it, especially about how lifestyle changes can affect your symptoms. Exercising and losing weight if you're overweight are important ways to lessen the joint pain and stiffness of osteoarthritis.
- Exercise. Low-impact exercise can increase your endurance and strengthen the muscles around your joint, making your joint more stable. Try walking, bicycling or water aerobics. If you feel new joint pain, stop.
- Lose weight. Carrying extra weight increases the stress on your weight-bearing joints, such as your knees and your hips. Even minor weight loss can relieve some pressure and reduce pain. Talk to a dietitian about healthy ways to lose weight.
Other things to try include:
- Movement therapies. Tai chi and yoga involve gentle exercises and stretches combined with deep breathing. Many people use these therapies to reduce stress in their lives. And research suggests that tai chi and yoga might reduce osteoarthritis pain and improve movement. Make sure the yoga you choose is a gentle form and that your instructor knows which of your joints are affected. Avoid moves that cause pain in your joints.
- Heat and cold. Both heat and cold can relieve pain and swelling in your joint. Heat, especially moist heat, can help muscles relax and ease pain. Cold can relieve muscle aches after exercise and decrease muscle spasms.
- Capsaicin. Capsaicin is a chili pepper extract. Applying capsaicin cream to your skin over a painful arthritic joint might help the pain. You might have to apply it 3 to 4 times a day for several weeks before you see a benefit. Capsaicin causes a burning or stinging feeling. Wash your hands well after applying capsaicin cream.
- NSAID gels. Topical nonsteroidal anti-inflammatory gel is available without a prescription. These gels may help relieve pain when applied to the skin over the affected joint.
- Braces or shoe inserts. Shoe inserts or other devices might help reduce pain when you stand or walk. These devices can support your joint to help take pressure off the joint.
-
Assistive devices. Assistive devices can help relieve stress on your joints. A cane or walker take weight off your knee or hip as you walk. Hold the cane in the hand opposite the leg that hurts.
Tools for gripping and grabbing may make it easier to work in the kitchen if you have osteoarthritis in your fingers. Check catalogs or medical supply stores or ask your healthcare team about assistive devices.
Alternative medicine
Complementary and alternative medicine treatments that have shown promise for osteoarthritis include:
- Acupuncture. Some studies indicate that acupuncture can relieve pain and improve function in people who have knee osteoarthritis. During acupuncture, hair-thin needles are inserted into your skin at precise spots on your body.
- Glucosamine and chondroitin. Studies have been mixed on these nutritional supplements. A few have found benefits for people with osteoarthritis, while most indicate that these supplements work no better than a placebo.
- Omega-3 fatty acids. Omega-3s, found in fatty fish and fish oil supplements, might help relieve pain and improve function.
Talk to your healthcare team about supplements you're considering.
Coping and support
Your ability to cope despite pain and disability caused by osteoarthritis often determines how much of an impact osteoarthritis has on your life. Talk to your healthcare team if you're feeling frustrated. Your care team may have ideas to help you cope or be able to refer you to someone who can help.
Preparing for your appointment
You might start by seeing your primary healthcare professional, who might refer you to a doctor who specializes in joint conditions, called a rheumatologist, or to an orthopedic surgeon.
What you can do
Make a list that includes:
- Detailed descriptions of your symptoms and when they began.
- Information about medical conditions you, your parents and your siblings have had.
- All the prescription and over-the-counter medicines and dietary supplements you take and the doses.
- Questions to ask the care team.
What to expect from your doctor
Your healthcare professional might ask some of the following questions:
- Is the pain continuous, or does it come and go?
- Do any particular activities make the pain better or worse?
- Have you ever injured this joint?

