Diagnosis
Mouth cancer FAQs
Oncologist Katharine Price, M.D., answers common questions about mouth cancer, which is also called oral cancer.
Hi. I'm Dr. Katharine Price at Mayo Clinic, and I'm here to answer some of the important questions you may have about oral cancer.
There are several things that you can do to prevent oral cancer. The most important is not to use any tobacco. It is also important not to drink too much alcohol or to abstain from alcohol altogether. A very simple thing that everyone can do that will decrease the risk of oral cancer is increase fruit and vegetable consumption. It's very important to try and reduce stress and to exercise on a regular basis.
So as a cancer doctor, I'm commonly asked what is my chance of cure? And that's a very difficult question because there is no absolute time point where we can say that you are cured of your cancer. But for oral cancer, most of the cancers will come back within the first two years of treatment. And if somebody gets to five years after treatment with no sign of cancer, the chance of it coming back is very, very low. So in general, we think about a five-year mark after cancer treatment as being cured. But again, it is not an absolute cut-off and sometimes we'll see recurrences beyond that point. But it is very unlikely.
It is very important for all patients to know that mental illness after or during a diagnosis of oral cancer is very common. The most common things that we'll see are depression and anxiety. Depression is very common, particularly when patients are going through treatment or immediately afterwards where they still have a lot of symptoms that they're trying to recover from. Anxiety would be the most common thing that we see. Because a diagnosis of cancer highlights the uncertainty of the future. None of us know what the future holds. None of us know if we're going to survive tomorrow or a year or 10 years from now. But having a cancer diagnosis really brings that to the forefront. What is really important for patients to know is that help is available. That help can take a lot of different forms, from medications to therapy to alternative treatments.
If you happen to be taking care of somebody who has oral cancer and is going through oral cancer treatment, the most important thing that you can do is show up and be there for them in a general sense. There's a lot of things that are impacted when somebody goes through oral cancer treatment. Some of the things that we do every day are hard: eating, sleeping, speaking. They may have pain. They may have side effects from treatment. And unfortunately, as a caregiver, you can't take any of those things away, but you can be supportive in a general sense and just be there with them. Know that you can't fix it, but that you can walk on that pathway with them so that they're not alone.
When someone is going through cancer treatment, your medical team does not expect you to pretend like everything's okay or put on a happy face. We know that you're going through difficult problems and we know that the treatment that we're having you do can be very difficult and cause a lot of symptoms. So the single most important thing is to communicate with your team, to let them know how you're doing. Never hesitate to ask your medical team any questions or concerns you have. Being informed makes all the difference. Thanks for your time and we wish you well.
Mouth cancer diagnosis might start with an exam of the lips and mouth. A healthcare professional might remove a sample of tissue for testing to see if you have mouth cancer.
Mouth cancer exam
Leukoplakia
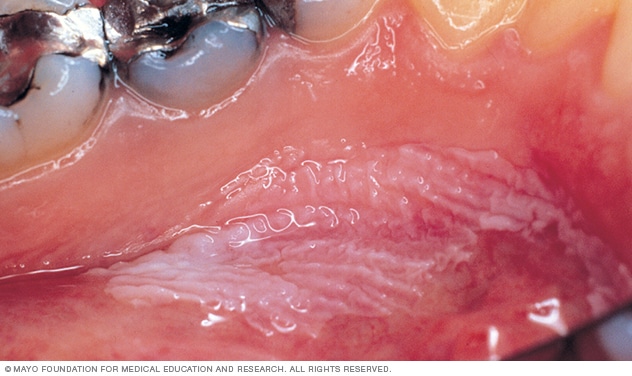
Leukoplakia
Leukoplakia appears as thick, white patches on the inside surfaces of the mouth. It has several possible causes, including repeated injury or irritation. It also can be a sign of mouth cancer or a sign of changes that could lead to cancer.
In a physical exam for mouth cancer, a healthcare professional looks at and feels your lips and mouth. That person checks for any lumps and areas of irritation. White patches in the mouth, called leukoplakia, and sores may be early signs of cancer.
Mouth cancer biopsy
If something concerning is found in an exam, the next step might be a mouth cancer biopsy. A biopsy is a procedure to remove a sample of tissue for testing in a lab. For a mouth cancer biopsy, a healthcare professional may use a cutting tool to cut away some concerning tissue from the mouth.
In the lab, tests can check the tissue for signs of cancer. Other tests might look for changes in the DNA inside the cancer cells. Results from these tests may help your healthcare team make a treatment plan.
Mouth cancer staging
Your healthcare team may do other tests to see if the cancer has spread beyond the mouth. Your healthcare team may use the results of these tests to give your cancer a stage. The stage tells your healthcare team about the extent of the cancer and about the prognosis. It also helps guide the treatment plan.
Mouth cancer staging tests may include:
- Using a small camera to look at the throat. During a procedure called endoscopy, a healthcare professional passes a thin, flexible tube equipped with a camera down the throat. The procedure helps the health professional look for signs that cancer has spread beyond the mouth.
- Imaging tests. A variety of imaging tests may help check whether cancer has spread beyond the mouth. Imaging tests may include X-ray, CT, MRI and positron emission tomography scans, also called PET scans. Not everyone needs each test. Your healthcare team decides which tests are needed based on your condition.
Mouth cancer stages range from 0 to 4. The lowest stages mean the cancer is small and hasn't grown very deep into the tissue in the mouth. As the cancer grows larger and grows deeper into the tissue, the stages get higher. A stage 4 mouth cancer can mean the cancer has grown very large or has spread to the lymph nodes. Stage 4 mouth cancer also can mean the cancer has spread to other parts of the body.
More Information
Treatment
Treatments for mouth cancer include surgery, radiation therapy and medicines. Medicines that help treat mouth cancer include chemotherapy, targeted therapy and immunotherapy. You may have just one type of treatment, or you may undergo a combination of cancer treatments.
Your healthcare team considers many factors when creating a mouth cancer treatment plan. These may include the cancer's location and how fast it's growing. The team also may look at whether the cancer has spread to other parts of the body and the results of tests on the cancer cells. Your team also considers your overall health and personal preferences.
Surgery to remove mouth cancer
During mouth cancer surgery, the surgeon removes the cancer and some of the healthy cells around it, called a margin. Removing the margin helps ensure that all the cancer cells are removed. The extent of the surgery depends on the size of the cancer. If cancer has spread into bone, the surgeon may remove some bone tissue.
Surgery carries a risk of bleeding and infection. Surgery for mouth cancer may affect your appearance. It also may affect the ability to speak, eat and swallow. Physical therapy and other rehabilitation services can help you cope with these changes.
You may need a tube to help you eat, drink and take medicine. For short-term use, the tube may be inserted through the nose and into the stomach. Longer term, a tube may be inserted through the skin and into the stomach.
Surgery to reconstruct the mouth
Reconstructive surgery may be needed when parts of the face, jaw or neck are removed during surgery. Healthy bone or tissue may be taken from other parts of the body and used to fill gaps left by the cancer. This tissue can replace part of the lip, tongue, palate or jaw, face, throat, or skin. Dental implants also may be used to replace your natural teeth.
If reconstruction is used to replace parts of the mouth, it usually is done at the same time as surgery to remove the cancer.
Surgery to remove lymph nodes in the neck
When mouth cancer spreads, it often goes to the lymph nodes in the neck first. If there are signs that the cancer has spread to the lymph nodes, you might need surgery to remove some lymph nodes, called a neck dissection. Even if there are no signs of cancer in the lymph nodes, you may have some of them removed as a precaution. Removing the lymph nodes removes the cancer and helps your healthcare team decide if you need other treatments.
To get to the lymph nodes, the surgeon makes a cut in the neck and removes the lymph nodes through the opening. The lymph nodes are tested for cancer. If cancer is found in the lymph nodes, other treatment might be needed to kill any cancer cells that are left. Options might include radiation or radiation combined with chemotherapy.
Sometimes the surgeon will remove only a few lymph nodes for testing. This is called a sentinel lymph node biopsy. In a sentinel lymph node biopsy, the surgeon removes the first few nodes into which a cancer may have spread. The lymph nodes are tested for cancer. If there's no cancer detected, it's likely that the cancer hasn't spread. Sentinel node biopsy isn't an option for everyone with mouth cancer. It's only used in some situations.
Radiation therapy for mouth cancer
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources. Radiation therapy for mouth cancer is most often delivered by a machine that moves around the body. The machine aims radiation to precise points. This kind of radiation therapy is called external beam radiation.
Sometimes radiation therapy for mouth cancer involves placing radioactive material inside the body. This kind of radiation therapy is called brachytherapy.
Radiation therapy might be the only treatment needed if the mouth cancer is very small. More often, radiation therapy is used after surgery. It can help kill any cancer cells that might remain. Sometimes radiation therapy may be combined with chemotherapy. This combination increases the effectiveness of radiation therapy. It also increases the risk of side effects.
If the cancer grows large or spreads to other parts of the body, radiation therapy may help relieve pain and other symptoms caused by the cancer.
The side effects of radiation therapy to the mouth may include dry mouth, tooth decay and damage to the jawbone.
You may need to see a dentist before radiation therapy starts to be sure your teeth are as healthy as possible. Any unhealthy teeth may need treatment or removal. A dentist can also help you understand how best to care for your teeth during and after radiation therapy to reduce your risk of complications.
Chemotherapy for mouth cancer
Chemotherapy treats cancer with strong medicines. Chemotherapy is often used after surgery to kill any cancer cells that remain. Chemotherapy may increase the effectiveness of radiation therapy, so the two treatments are often combined. If the cancer spreads to other parts of the body, chemotherapy can help control it.
The side effects of chemotherapy depend on which medicines you receive. Common side effects include nausea, vomiting and hair loss. Ask your healthcare team which side effects are likely for the chemotherapy medicines you'll receive.
Targeted therapy for mouth cancer
Targeted therapy for cancer is a treatment that uses medicines to attack specific chemicals in the cancer cells. By blocking these chemicals, targeted therapy can cause cancer cells to die.
For mouth cancer, targeted therapy may be used alone or in combination with chemotherapy or radiation therapy. It might be used after surgery to kill any cancer cells that remain. It also can help control a cancer that comes back or that spreads to other parts of the body.
Immunotherapy for mouth cancer
Immunotherapy for cancer is a treatment with medicine that helps the body's immune system kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn't be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells.
For mouth cancer, immunotherapy might be used when mouth cancer comes back or spreads to other parts of the body.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Quit using tobacco
Mouth cancers are closely linked to tobacco use, including cigarettes, cigars, pipes, chewing tobacco and snuff, among others. Not everyone who is diagnosed with mouth cancer uses tobacco. But if you do, now is the time to stop because:
- Tobacco use makes treatment less effective.
- Tobacco use makes it harder for the body to heal after surgery.
- Tobacco use increases the risk of a cancer recurrence and of getting another cancer in the future.
Quitting smoking or chewing can be very difficult. And it's that much harder when you're trying to cope with a stressful situation, such as a cancer diagnosis and treatment. Talk with your healthcare team about your options. This might include medicines, nicotine replacement products and counseling.
Quit drinking alcohol
Alcohol, particularly when combined with tobacco use, greatly increases the risk of mouth cancer. If you drink alcohol, stop drinking all types of alcohol. This may help reduce your risk of a second cancer.
Alternative medicine
No alternative medicine treatments have been found to cure mouth cancer. But complementary and alternative medicine treatments may help you cope with mouth cancer and the side effects of cancer treatment, such as fatigue.
Many people with mouth cancer have fatigue during and after treatment. The feeling of being very tired and worn down can continue for years. When combined with care from your healthcare team, complementary and alternative medicine may help relieve fatigue.
Talk with your healthcare team about:
Gentle exercise
If you get the OK from your healthcare team, start with gentle exercise. Add more exercise as you feel up to it. Consider walking, swimming, yoga and tai chi.
Managing stress
Take control of stress in your daily life. Try stress-reduction techniques such as muscle relaxation or visualization. Writing in a journal also may help.
Massage therapy
During a massage, a massage therapist applies pressure to your skin and muscles. Some massage therapists are specially trained to work with people who have cancer. Ask your healthcare team for names of massage therapists in your community.
Acupuncture
During an acupuncture session, a trained practitioner inserts thin needles into precise points on your body. Some acupuncturists are specially trained to work with people with cancer. Ask your healthcare team to recommend someone in your community.
Coping and support
As you talk about your mouth cancer treatment options with your healthcare team, it's common to feel overwhelmed. People who are newly diagnosed with mouth cancer may be trying to cope with the diagnosis at the same time they need to make decisions about their treatment. Here are some ideas that may help.
Learn enough about mouth cancer to make treatment decisions
Make a list of questions to ask at your next appointment. Bring someone along to help you take notes. Ask your healthcare team about reliable books or websites to turn to for accurate information. The more you know about your cancer and your treatment options, the more confident you may feel as you make treatment decisions.
Find a good listener
Finding someone who is willing to listen to you talk about your hopes and fears can be helpful as you manage a cancer diagnosis. This could be a friend or family member. A counselor, medical social worker or clergy member also may offer helpful guidance and care.
Talk to other mouth cancer survivors
Other people with mouth cancer may understand what you're going through. Ask your healthcare team about support groups for people with cancer in your community. In the United States, contact your local chapter of the American Cancer Society. Another option is online support groups, such as those run by the Oral Cancer Foundation.
Take time for yourself
Set aside time for yourself each day. Use this time to take your mind off your cancer and do what makes you happy. Even a short break to relax in the middle of a day full of tests and appointments may help you cope.
Preparing for your appointment
Make an appointment with a doctor, dentist or other healthcare professional if you have symptoms that worry you.
If your healthcare professional feels that you may have mouth cancer, you may be referred to a periodontist or otolaryngologist. A periodontist is a dentist who specializes in diseases of the gums and related tissue in the mouth. An otolaryngologist is a doctor who specializes in diseases that affect the ears, nose and throat.
Appointments can be brief, so it's a good idea to be prepared. Here's some information to help you get ready, and what to expect.
What you can do
- Be aware of anything you need to do to prepare. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as change your diet.
- Write down any symptoms you have, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements you're taking and the doses.
- Consider bringing a trusted person along. Sometimes it can be hard to remember all the information provided during an appointment. Someone who comes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Write down questions to ask your doctor
Your time with your healthcare team is limited, so prepare a list of questions to make the most of your time together. List your questions from most important to least important in case time runs out. For mouth cancer, some basic questions to ask your doctor include:
- What may be causing my symptoms or condition?
- What kinds of tests do I need?
- What do you recommend for next steps in determining my diagnosis and treatment?
- What are the alternatives to the approach that you're suggesting?
- Do I need to start treatment right away?
- What are the possible side effects of treatment?
- I have these other health conditions. How can I best treat them together?
- Are there any restrictions that I need to follow?
- Should I see a specialist?
- Where can I find more information?
In addition to the questions that you've prepared, don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your healthcare team is likely to ask you questions, such as:
- When did you first begin experiencing symptoms?
- How have your symptoms changed over time?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Do you now or have you ever used tobacco?
- Do you drink alcohol?
- Have you ever received radiation therapy to your head or neck area?
Jan. 16, 2025