Diagnosis
Excisional biopsy
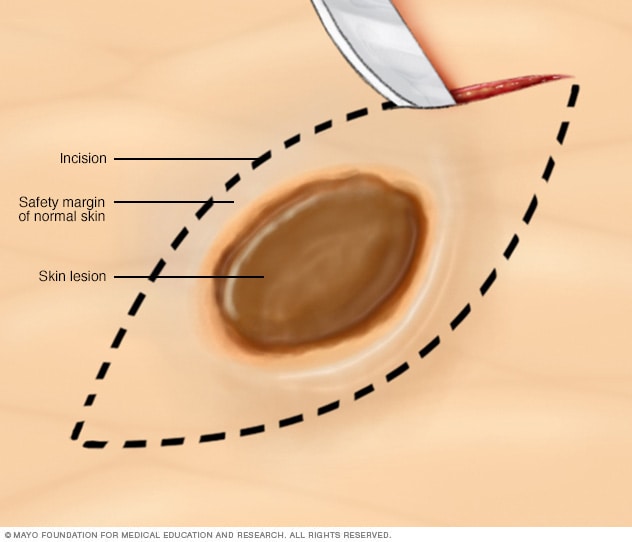
Excisional biopsy
During an excisional biopsy, a scalpel is used to cut out a lump or an area of irregular skin and some surrounding healthy skin. As a rule, stitches are needed to close the wound.
Punch biopsy
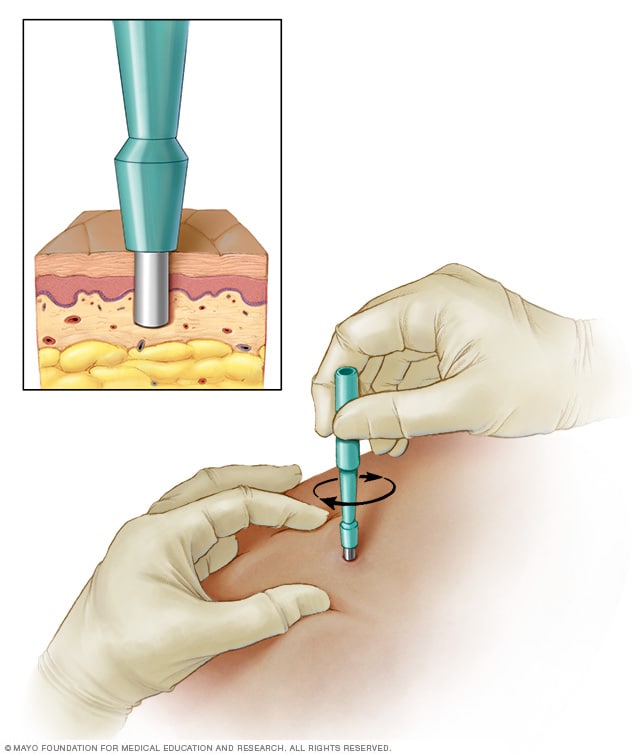
Punch biopsy
During a punch biopsy, a round-tipped cutting tool is used to remove deeper layers of skin for testing. Depending on the size, stitches may be needed to close the wound.
Tests and procedures used to diagnose melanoma include:
Physical exam
Your healthcare professional will ask questions about your health history. That person also will examine your skin to look for signs that could mean melanoma.
Removing a sample of tissue for testing
A biopsy is a procedure to remove a sample of tissue for testing in a lab. What type of biopsy procedure is used depends on your situation. Most often healthcare professionals recommend removing the entire growth when possible.
One common technique is called the punch biopsy. A punch biopsy is done with a circular blade that's pressed into the skin around the suspicious mole.
Another technique is called an excisional biopsy. An excisional biopsy uses a scalpel to cut away the entire mole and some of the healthy tissue around it.
Determining the extent of the melanoma
Related information
Melanoma spread: How lymph nodes play a role in detection
If you receive a diagnosis of melanoma, the next step is to determine the extent of the cancer, called the stage. To assign a stage to your melanoma, your healthcare team will:
-
Determine the thickness. In general, the thicker the melanoma, the more serious the disease. The thickness of a melanoma is determined by looking at the melanoma under a microscope and measuring it with a special tool. The thickness of a melanoma helps your care team decide on a treatment plan.
Thinner melanomas may only require surgery to remove the cancer and some healthy tissue around it. If the melanoma is thicker, your healthcare team may recommend more tests to see if the cancer has spread before deciding on your treatment options.
-
See if the melanoma has spread to the lymph nodes. If there's a risk that the cancer has spread to nearby lymph nodes, you might need a sentinel node biopsy.
During a sentinel node biopsy, a dye is injected in the area where your melanoma was removed. The dye flows to the nearby lymph nodes. The first lymph nodes to take up the dye are removed and tested for cancer cells. These first lymph nodes are called the sentinel lymph nodes. If they're cancer-free, there's a good chance that the melanoma has not spread.
- Look for signs of cancer beyond the skin. If there is concern that the melanoma has spread, imaging tests might be used to look for signs of cancer in other areas of the body. Tests might include X-ray, MRI, CT and positron emission tomography, which is also called a PET scan. These imaging tests generally aren't used for smaller melanomas with a lower risk of spreading beyond the skin.
Other factors may go into determining the risk that the cancer may spread. One factor is whether the skin over the area has formed an open sore, called ulceration. Another is how many dividing cancer cells are found when looking at a sample of the cancer under a microscope. Doctors call this the cancer's mitotic rate.
Your healthcare team uses the results from these tests to figure out your melanoma's stage. Melanoma stages use the numbers 0 through 4. At stage 0 and stage 1, a melanoma is thin and small. Treatment is likely to be successful. As the melanoma grows deeper into the skin, the stages get higher. Treatment becomes more challenging. By stage 4, the cancer has spread beyond the skin to other organs, such as the lungs or liver.
Treatment
Melanoma treatment often starts with surgery to remove the cancer. Other treatments may include radiation therapy and treatment with medicine. Treatment for melanoma depends on several factors. These factors include the stage of your cancer, your overall health and your own preferences.
Surgery
Treatment for melanoma usually includes surgery to remove the melanoma. A very thin melanoma may be removed entirely during the biopsy and require no further treatment. Otherwise, your surgeon will remove the cancer as well as some of the healthy tissue around it.
For people with melanomas that are small and thin, surgery might be the only treatment needed. If the melanoma has grown deeper into the skin, there might be a risk that the cancer has spread. So other treatments are often used to make sure all the cancer cells are killed.
If the melanoma has grown deeper into the skin or if it may have spread to the nearby lymph nodes, surgery might be used to remove the lymph nodes.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources. During radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body.
Radiation therapy may be directed to the lymph nodes if the melanoma has spread there. Radiation therapy also can be used to treat melanomas that can't be removed completely with surgery. For melanoma that spreads to other areas of the body, radiation therapy can help relieve symptoms.
Immunotherapy
Immunotherapy for cancer is a treatment with medicine that helps the body's immune system to kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn't be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells.
For melanoma, immunotherapy may be used after surgery for cancer that has spread to the lymph nodes or to other areas of the body. When melanoma can't be removed completely with surgery, immunotherapy treatments might be injected directly into the melanoma.
Targeted therapy
Targeted therapy for cancer is a treatment that uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die.
For melanoma, targeted therapy might be recommended if the cancer has spread to your lymph nodes or to other areas of your body. Cells from your melanoma may be tested to see if targeted therapy is likely to be effective against your cancer.
Chemotherapy
Chemotherapy treats cancer with strong medicines. Many chemotherapy medicines exist. Most are given through a vein. Some come in pill form.
Chemotherapy might be an option to help control melanoma that doesn't respond to other treatments. It might be used when immunotherapy or targeted therapy aren't helping.
Sometimes chemotherapy can be given in a vein in your arm or leg in a procedure called isolated limb perfusion. During this procedure, blood in your arm or leg isn't allowed to travel to other areas of your body for a short time. This helps keep the chemotherapy medicines near the melanoma and doesn't affect other parts of your body.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
With time, you'll find what helps you cope with the uncertainty and distress of a cancer diagnosis. Until then, you may find it helps to:
Learn enough about melanoma to make decisions about your care
Ask your healthcare team about your cancer, including your test results, treatment options and, if you like, your prognosis. As you learn more about melanoma, you may become more confident in making treatment decisions.
Keep friends and family close
Keeping your close relationships strong will help you deal with your melanoma. Friends and family can provide the practical support you'll need, such as helping take care of your home if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by having cancer.
Find someone to talk with
Find someone who is willing to listen to you talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Ask your healthcare team about support groups in your area. Other sources of information include the National Cancer Institute and the American Cancer Society.
Preparing for your appointment
Make an appointment with a doctor or other healthcare professional if you notice any skin changes that worry you.
If your healthcare professional thinks you might have melanoma, you may be referred to a doctor who specializes in skin diseases. This doctor is called a dermatologist. If a cancer diagnosis is made, you also may be referred to a doctor who specializes in treating cancer. This doctor is called an oncologist.
Because appointments can be brief, it's a good idea to be prepared. Here's some information to help you get ready.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down symptoms you're experiencing, including any that may not seem related to the reason for which you scheduled the appointment.
- Write down key personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements you're taking and the doses.
- Take a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your healthcare team.
Your time with your healthcare team is limited, so prepare a list of questions to help you make the most of your time together. List your questions from most important to least important in case time runs out. For melanoma, some basic questions to ask include:
- Do I have melanoma?
- How large is my melanoma?
- How deep is my melanoma?
- Has my melanoma spread beyond the area of skin where it was first discovered?
- What additional tests do I need?
- What are my treatment options?
- Can any treatment cure my melanoma?
- What are the potential side effects of each treatment option?
- Is there one treatment you feel is best for me?
- How long can I take to decide on a treatment option?
- Should I see a specialist? What will that cost, and will my insurance cover it?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
- What will determine whether I should plan for a follow-up visit?
Don't hesitate to ask other questions.
Dec. 30, 2023