Diagnosis
Before infertility testing, your health care team or clinic works to understand your sexual habits. They might make recommendations to improve your chances of getting pregnant. But in some infertile couples, no clear cause is found. That is called unexplained infertility.
Infertility testing can involve uncomfortable procedures. It can be expensive too. And some medical plans may not cover the cost of fertility treatment. Also, there's no guarantee that you'll get pregnant — even after all the testing and counseling.
Tests for men
Male fertility relies on the testicles making enough healthy sperm. The sperm needs to be released from the penis into the vagina, where it has to travel to the waiting egg. Tests for male infertility try to find out whether there are treatable problems with any of these steps.
You may have a physical exam that includes a check of your genitals. Specific infertility tests may include:
- Semen analysis. Your health care team may ask for one or more samples of your semen. Often, you collect semen by masturbating or by stopping sex to ejaculate into a clean container. Then a lab checks your semen sample. In some cases, urine may be tested to find out if it contains sperm.
- Hormone testing. You may get a blood test to check your level of testosterone and other male hormones.
- Genetic testing. This may be done to find out whether a genetic defect is the cause of infertility.
- Testicular biopsy.This procedure removes a small amount of testicle tissue so a lab can check it under a microscope. It's not common to need a biopsy during infertility testing. Rarely, it may be done to find out whether there is a blockage in the reproductive tract that keeps sperm from leaving the body in semen. Most of the time, this diagnosis can be made based on your history, physical exam and lab tests. Other times, a biopsy may be done to find conditions that contribute to infertility. Or it may be used to collect sperm for assisted reproductive techniques, such as in vitro fertilization (IVF).
- Imaging. In some cases, your health care team may recommend tests that make pictures of the inside of your body. For example, ultrasound can check for problems in the scrotum, in the glands that make fluids that become semen or in the tube that carries sperm out of the testicles. A brain MRI can check for tumors of the pituitary gland that are not cancer. These tumors can cause the gland to make too much of the hormone prolactin, which could lead the body to make less sperm or none.
- Other testing. In rare cases, other tests may be done to check the quality of your sperm. For example, a semen sample may need to be checked for problems with DNA that might damage sperm.
Tests for women
Hysterosonography
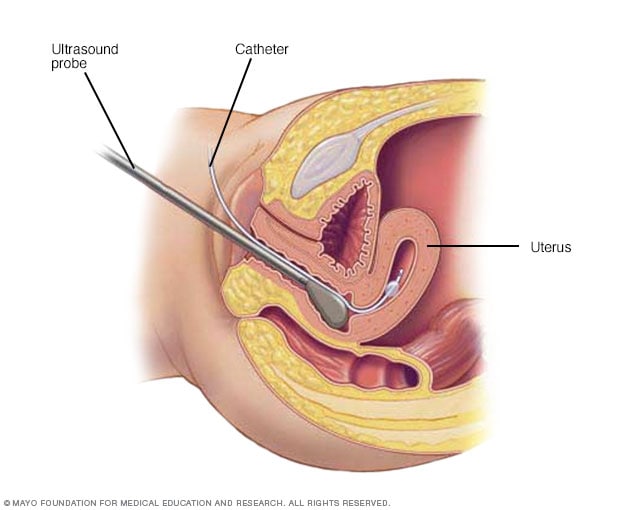
Hysterosonography
During hysterosonography (his-tur-o-suh-NOG-ruh-fee), you have a thin, flexible tube called a catheter placed in the uterus. Salt water, also called saline, is injected through the flexible tube into the hollow part of the uterus. An ultrasound probe transmits images of the inside of the uterus to a nearby monitor.
Hysteroscopy
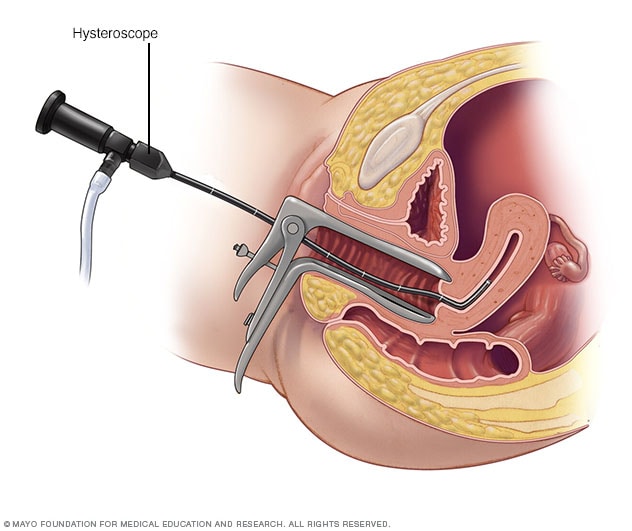
Hysteroscopy
During hysteroscopy (his-tur-OS-kuh-pee), a thin, lighted instrument provides a view of the inside of the uterus. This instrument also is called a hysteroscope.
Video: HSG test for female infertility
Blocked fallopian tubes or an abnormal uterine cavity may cause infertility.
Hysterosalpingography, or HSG, is an X-ray test to outline the internal shape of the uterus and show whether the fallopian tubes are blocked.
In HSG, a thin tube is threaded through the vagina and cervix. A substance known as contrast material is injected into the uterus.
A series of X-rays, or fluoroscopy, follows the dye, which appears white on X-ray, as it moves into the uterus and then into the tubes. If there is an abnormality in the shape of the uterus, it will be outlined.
If the tube is open, the dye gradually fills it. The dye spills into the pelvic cavity, where the body resorbs it.
Fertility for women relies on the ovaries releasing healthy eggs. The reproductive tract must let an egg pass into the fallopian tubes and join with sperm. Then the fertilized egg must travel to the uterus and attach to the lining. Tests for female infertility try to find problems with any of those steps.
You may have a physical exam, including a regular pelvic exam. Infertility tests may include:
- Ovulation testing. A blood test measures hormone levels to find out whether you're ovulating.
- Thyroid function test. This blood test can be done if your health care team thinks your infertility might be related to a problem with the thyroid gland. If the gland makes too much or little thyroid hormone, that could play a role in fertility trouble.
- Hysterosalpingography. Hysterosalpingography (his-tur-o-sal-ping-GOG-ruh-fee) checks on the condition of the uterus and fallopian tubes. It also looks for blockages in the fallopian tubes or other problems. Special dye is injected into the uterus, and an X-ray is taken.
- Ovarian reserve testing. This helps your care team find out how many eggs you have for ovulation. The method often begins with hormone testing early in the menstrual cycle.
- Other hormone tests. These check the levels of hormones that control ovulation. They also check pituitary hormones that control processes involved in having a baby.
- Imaging tests. Pelvic ultrasound looks for diseases of the uterus or ovaries. Sometimes a test called a saline infusion sonogram is used to see details inside the uterus that can't be seen on a regular ultrasound. Another name for the saline infusion test is a sonohysterogram (son-o-his-ter-OH-gram).
Rarely, testing may include:
- Hysteroscopy. Depending on your symptoms, your health care team may use a hysteroscopy (his-ter-os-ko-pee) to look for a disease of the uterus. During the procedure, a thin, lighted device is placed through the cervix into the uterus to check for any irregular signs. It also can help guide minor surgery.
- Laparoscopy. Laparoscopy (lap-u-ros-kuh-pee) involves a small cut beneath the navel. Then a thin viewing device is placed through the cut to check the fallopian tubes, ovaries and uterus. The procedure may find endometriosis, scarring, blockages or other issues with the fallopian tubes. It also might find treatable problems with the ovaries and uterus. Laparoscopy is a type of surgery that can treat certain conditions as well. For example, it can be used to remove growths called fibroids or endometriosis tissue.
Not everyone needs to have all, or even many, of these tests before the cause of infertility is found. You and your health care team decide which tests you will have and when.
Treatment
Infertility treatment depends on:
- The cause of the infertility.
- How long you've been infertile.
- Your age and your partner's age, if you have a partner.
- Personal preferences.
Some causes of infertility can't be corrected.
If pregnancy doesn't happen after a year of unprotected sex, couples often can still become pregnant through infertility treatments called assisted reproductive technology. But treatment can involve big financial, physical, emotional and time commitments.
Treatment for men
Men's treatment for general sexual problems or a lack of healthy sperm may include:
- Lifestyle changes. Your health care team may recommend that you take the following steps. Have sex more often and closer to the time of ovulation. Get regular exercise. Drink less alcohol or give up harmful substances such as tobacco. Stop taking medicines that can affect fertility, but only if your health care team tells you to.
- Medicines. Your team may prescribe medicines to improve sperm count and boost the chances of a successful pregnancy. These prescription drugs may help the testicles function better too.
- Surgery. Sometimes, surgery may be able to reverse a sperm blockage and restore fertility. In other cases, repairing a large varicocele may improve the overall chances for pregnancy.
- Sperm retrieval procedures. These techniques can collect sperm if you can't ejaculate, or if no sperm is in your semen. Sperm retrieval procedures also may be used when assisted reproductive techniques are planned and sperm counts are low or irregular.
Treatment for women
Some women need only one or two treatments to improve fertility. Others may need a few types of therapies to become pregnant.
- Fertility medicines. These are the main treatments for infertility that's due to ovulation trouble. They can help the ovaries release an egg if ovulation is irregular or stops happening. Talk with your health care team about your options. Ask about the benefits and risks of each type of fertility medicine.
- Intrauterine insemination (IUI). With IUI, healthy sperm are placed directly in the uterus around the time that the ovary releases one or more eggs to be fertilized. Depending on the reasons for infertility, IUI can be timed with your menstrual cycle or with the use of fertility medicines. Your partner or a donor provides the sperm.
- Surgery to restore fertility. Some conditions of the uterus can be treated with hysteroscopy. These include polyps, scar tissue and some fibroids. Laparoscopic surgery with small cuts or traditional surgery with a large cut in the stomach area may be needed to treat conditions such as endometriosis, pelvic adhesions and larger fibroids.
Assisted reproductive technology
In vitro fertilization
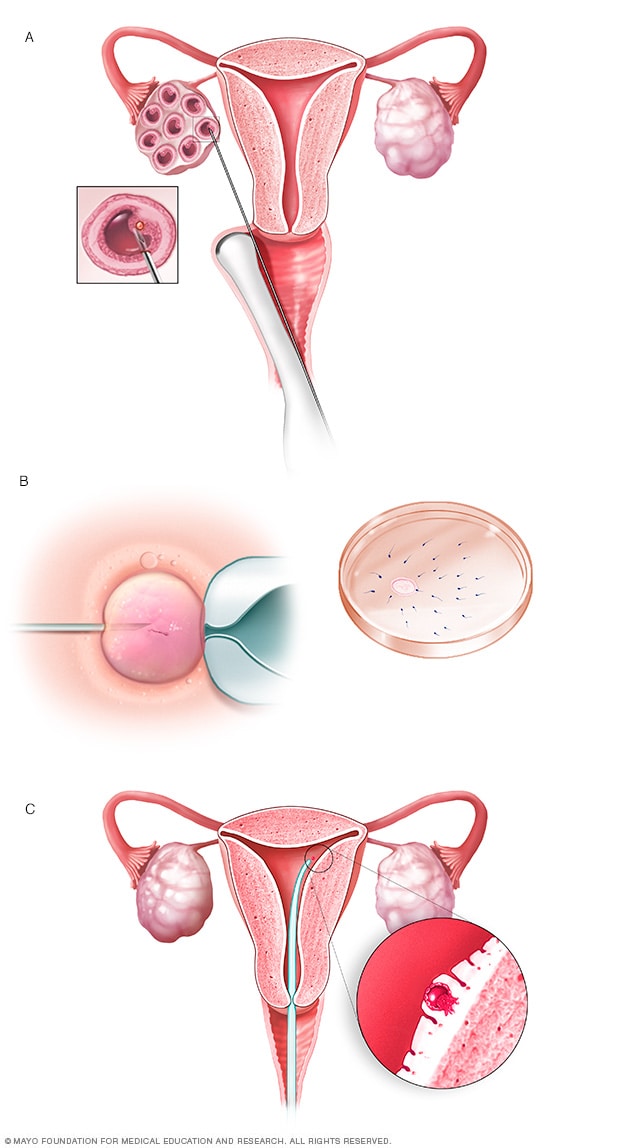
In vitro fertilization
During in vitro fertilization, eggs are removed from sacs called follicles within an ovary (A). An egg is fertilized by injecting a single sperm into the egg or mixing the egg with sperm in a petri dish (B). The fertilized egg, called an embryo, is transferred into the uterus (C).
ICSI
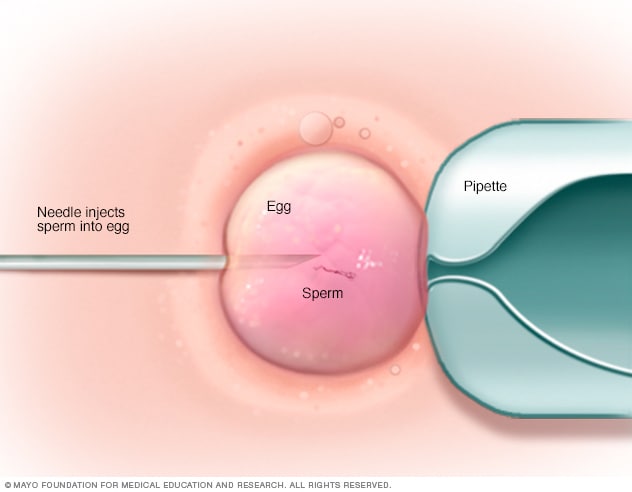
ICSI
In intracytoplasmic sperm injection (ICSI), a single healthy sperm is injected directly into each mature egg. ICSI often is used when semen quality or number is a problem or if fertilization attempts during prior in vitro fertilization cycles failed.
Assisted reproductive technology (ART) is any fertility treatment in which the egg and sperm are handled.
In vitro fertilization (IVF) is the most common ART technique. Some of the key steps in a cycle of IVF include:
- Fertility medicines are used to help the ovaries make eggs.
- Mature eggs are removed from the ovaries.
- The eggs are fertilized with sperm in a dish in a lab.
- The fertilized eggs, also called embryos, are placed in the uterus. Embryos also can be frozen for future use.
Sometimes, other techniques are used in an IVF cycle, such as:
- Intracytoplasmic sperm injection (ICSI). A single healthy sperm is injected directly into a mature egg. Often, ICSI is used when semen quality or quantity is poor. Or it might be used if fertilization attempts during prior IVF cycles didn't work.
- Assisted hatching. This technique helps an embryo attach to the lining of the uterus. It opens part of the outer covering of the embryo, which is why it's called hatching.
- Donor eggs or sperm. Often ART is done using a couple's own eggs and sperm. But you have the choice to use eggs or sperm from a donor. This is an option if you're single or in a same-sex relationship. It's also done for medical reasons. These include poor egg quality due to age and sperm problems such as a blockage in the reproductive tract. Donor eggs or sperm also might be used if one partner has a genetic disease that could be passed on to a baby. An infertile couple can use donated embryos too. These come from other couples who received infertility treatment and had leftover embryos that were frozen.
- Gestational carrier. People who don't have a working uterus or for whom pregnancy poses a serious health risk might choose IVF using a gestational carrier. In this case, the couple's embryo is placed in the uterus of a person who agrees to carry the pregnancy.
- Genetic testing. Embryos made with IVF can be tested for genetic problems. This is called preimplantation genetic testing. Embryos that don't seem to have a gene problem can be placed in the uterus. This lowers the risk of a parent passing on a genetic condition to a child.
Complications of treatment
Complications of infertility treatment may include:
- Multiple pregnancy. The most common complication of infertility treatment is a multiple pregnancy — twins, triplets or more. A higher number of unborn babies in the womb raises the risk of premature labor and delivery. It also makes problems during pregnancy more likely, such as gestational diabetes. Babies born too early face worse odds of health and development challenges. Ask your health care team about all the risks of a multiple pregnancy before you start treatment.
- Ovarian hyperstimulation syndrome (OHSS). Fertility medicines can cause this condition in which the ovaries become swollen and painful. The risk of OHSS goes up with the use of assisted reproductive technologies such as in vitro fertilization. Symptoms can include mild pain in the stomach area, bloating and upset stomach that lasts about a week. Nausea may last longer if you become pregnant. Rarely, a more serious form of OHSS causes rapid weight gain and shortness of breath. This is an emergency that needs to be treated in the hospital.
- Bleeding or infection. Assisted reproductive technology or reproductive surgery comes with a risk of bleeding or infection.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
Coping with infertility can be very hard, because there are so many unknowns. The journey can take a serious emotional toll. These steps can help you cope:
- Be prepared. The uncertainty of infertility testing and treatments can be stressful. Ask your fertility doctor to explain the steps and prepare for each one.
- Set limits. Before you start treatment, decide which procedures and how many you can afford financially and accept emotionally. Infertility treatments may be expensive and often are not covered by insurance companies. What's more, a successful pregnancy usually depends on more than one attempt at treatment.
- Think about other options. You might need to use donor sperm or eggs, or a gestational carrier. You could also consider adopting a child or choosing to have no children. Think about these options as early as possible in the infertility evaluation. It may ease anxiety during treatment and feelings of hopelessness if you don't become pregnant.
- Seek support. You might want to join an infertility support group or talk with a counselor before, during or after treatment. It can help you carry on through the process and ease grief if your treatment doesn't work.
Managing stress during treatment
Try these tips to help take charge of stress during infertility treatment:
- Express yourself. Reach out to others. It can help you deal with emotions such as anger, sadness or guilt.
- Stay in touch with loved ones. Talk to your partner, family or friends. The best support often comes from loved ones and those closest to you.
- Find ways to ease stress. Some studies suggest that people who get help managing stress during infertility treatment with ART have slightly better results than those who don't get help. Take steps to lower the stress in your life before you try to become pregnant. For instance, you could learn mindfulness meditation, practice yoga, keep a journal or make time for other hobbies that relax you.
- Exercise, eat a balanced diet and get enough sleep. These and other healthy habits can improve your outlook and keep you focused on living your life.
Managing emotional effects of the outcome
You may have emotional challenges no matter your results:
- Not getting pregnant or having a miscarriage. The stress of not being able to have a baby can be awful even in the most loving, supportive relationships.
- Success. Even if fertility treatment is successful, it's common to have stress and fear of failure during pregnancy. If you've had depression or anxiety in the past, you're at higher risk of those mental health conditions coming back in the months after your child's birth.
- Multiple births. A successful pregnancy that results in multiple births can add stress during pregnancy and after delivery.
Get professional help from a therapist if the emotional impact of infertility treatment, pregnancy or parenthood becomes too heavy for you or your partner.
Preparing for your appointment
Depending on your age and health history, your usual health care professional may recommend a medical evaluation. A gynecologist, urologist or family doctor can help find out whether there's a problem that requires a specialist or clinic that treats infertility problems. In some cases, both you and your partner may need a full infertility evaluation.
What you can do
To get ready for your first appointment:
- Note details about your attempts to get pregnant. Write down details about when you started trying to conceive and how often you've had sex, especially around the midpoint of your menstrual cycle — the time of ovulation.
- Bring your key medical information. Include any other health conditions that you or your partner has, as well as information about any previous infertility evaluations or treatments.
- Make a list of any medicines, vitamins, herbs or other supplements you take. Include the amounts you take, called the doses, and how often you take them.
- Make a list of questions to ask your health care team. List the most important questions first in case time runs short.
For infertility, some basic questions to ask your care team include:
- What kinds of tests do we need to find out why we haven't conceived yet?
- What treatment do you recommend we try first?
- What side effects might that treatment cause?
- What are the chances of having multiple babies with the treatment?
- How many times might we need to try this treatment before we conceive?
- If the first treatment doesn't work, what will you recommend trying next?
- Are there any long-term complications linked with this or other infertility treatments?
Feel free to ask your health care professional to repeat information or to ask follow-up questions.
What to expect from your doctor
Be ready to answer questions that your health care professional asks. Your answers can help your doctor figure out what tests and treatments you may need.
Questions for couples
Some questions that you and your partner may be asked are:
- How long have you been trying to get pregnant?
- How often do you have sex?
- Do you use any lubricants during sex?
- Do either of you smoke?
- Do either of you use alcohol or recreational drugs? How often?
- Are either of you taking any medicines, dietary supplements or anabolic steroids?
- Have either of you been treated for any other medical conditions, including sexually transmitted infections?
Questions for men
Your health care professional may ask:
- Do you have any trouble putting on muscle, or do you take any substances to increase muscle mass?
- Do you ever notice a fullness in the scrotum, especially after you stand for a long time?
- Do you have any testicle pain or pain after ejaculation?
- Have you had any sexual challenges, such as trouble keeping an erection, ejaculating too soon, not being able to ejaculate or having less sexual desire?
- Have you conceived a child with any previous partners?
- Do you often take hot baths or steam baths?
Questions for the woman
Your health care professional may ask:
- At what age did you get your menstrual period?
- What are your cycles typically like? How regular, long and heavy are they?
- Have you ever been pregnant before?
- Have you been charting your cycles or testing for ovulation? If so, for how many cycles?
- What is your typical daily diet?
- Do you exercise? How often?
Sept. 13, 2023