Overview
Where eye melanoma occurs
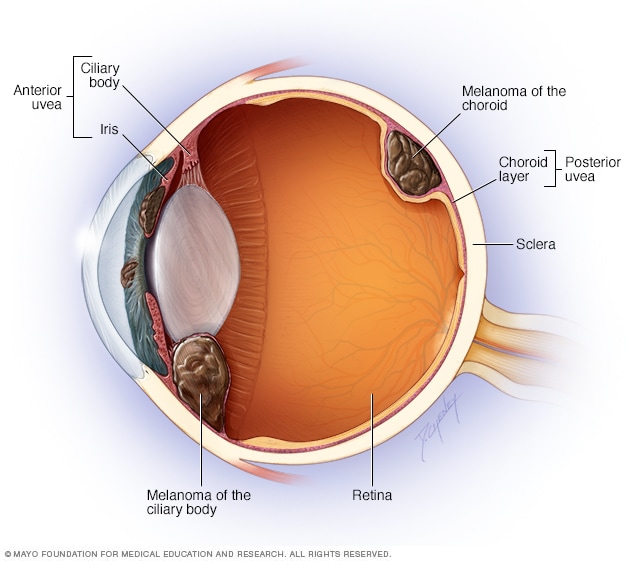
Where eye melanoma occurs
Eye melanoma most often affects the middle layer of the eye, called the uvea. Parts of the eye's uvea that can develop melanoma include the colored portion of the eye (iris), a structure around the eye's lens (ciliary body), and the layer of blood vessels that lines the back of the eye (choroid).
Eye melanoma is a kind of eye cancer that starts in cells within the eye that make melanin. Melanin is most often known as the pigment that gives skin its color. But the eyes have cells that make melanin too. Eye melanoma also is called ocular melanoma, intraocular melanoma and uveal melanoma.
Most eye melanomas form in parts of the eye you can't see when looking in a mirror. That makes eye melanoma hard to notice. And eye melanoma typically doesn't cause symptoms at first.
Eye melanoma can be treated. Treatment for small eye melanomas may not cause vision problems. But treatment for large eye melanomas typically leads to some vision loss.
Symptoms
Eye melanoma may not cause any symptoms. When they do happen, signs and symptoms of eye melanoma can include:
- Flashes of light or what look like specks of dust in a person's vision. These are sometimes called floaters.
- A growing dark spot in the colored part of the eye, called the iris.
- A change in the shape of the pupil. The pupil is the dark circle at the center of the eye.
- Poor vision or blurry vision in one eye.
- Not being able to see when looking to the side. This is called loss of peripheral vision.
When to see a doctor
Make an appointment with a healthcare professional if you have any symptoms of eye melanoma. If you notice sudden changes in your vision, seek emergency medical care right away.
Causes
It's not clear what causes eye melanoma.
Eye melanoma happens when cells in the eye develop changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do. In healthy cells, the DNA tells the cells to grow and multiply at a set rate. The DNA also tells the cells to die at a set time.
In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to grow and multiply quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells might form a mass called a tumor. The tumor can grow to invade and destroy healthy tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
Where eye melanoma develops
Eye melanoma most often happens in the cells of the middle layer of the eye, called the uvea. The uvea has three parts. Each part can be affected by eye melanoma:
- The iris. The iris is the colored part at the front of the eye.
- The choroid layer. The choroid layer is a layer of blood vessels and connective tissue. It's located at the back of the uvea.
- The ciliary body. The ciliary body is located behind the iris. It helps the eye focus. It also makes a transparent liquid, called aqueous humor, that fills the front part of the eye.
Eye melanoma can happen in other parts of the eye. But this is very rare. Other parts of the eye that can develop melanoma include:
- The layer on the front of the eye, called the conjunctiva.
- The socket that surrounds the eyeball, called the orbit.
- The eyelid.
Risk factors
Risk factors for eye melanoma include:
- Light eye color. People with blue eyes or green eyes have a higher risk of melanoma of the eye.
- Being white. White people have a greater risk of eye melanoma than do people of other races.
- Age. The risk of eye melanoma goes up with age.
-
Certain inherited skin conditions. A condition called dysplastic nevus syndrome, which causes unusual moles, can raise the risk of eye melanoma.
People who have a condition called ocular melanocytosis also are at higher risk of eye melanoma. This condition involves unusual skin pigmentation on the eyelids and in the tissue around the eyelids. It also leads to more pigmentation on the eye's uvea.
- Certain genetic changes. Some DNA changes that are passed from parents to children may raise the risk of eye melanoma.
- Exposure to ultraviolet light. Some research suggests that exposure to ultraviolet light could raise the risk of eye melanoma. Sources of ultraviolet light include the sun, as well as tanning beds.
Healthcare professionals haven't found anything that can prevent eye melanoma.
Complications
Some people develop other health concerns linked to eye melanoma. These are called complications. They can include the following:
Vision loss
Eye melanoma can cause vision loss. Sometimes the vision loss is a symptom of an eye melanoma. Sometimes vision loss is caused by eye melanoma treatment.
Eye melanoma that spreads beyond the eye
Eye melanoma can spread outside of the eye to other areas of the body, including the liver, lungs and bones.
Jan. 28, 2025