Overview
Esophagitis is swelling and irritation, called inflammation, of the tissues that line the esophagus. The esophagus is the muscular tube that carries food and drink from the mouth to the stomach.
Esophagitis (uh-sof-uh-JIE-tis) can cause painful, difficult swallowing. It also can lead to chest pain. Various things can cause esophagitis. Some common causes include stomach acids backing up into the esophagus, infection, medicines taken by mouth and allergies.
Treatment for esophagitis depends on its exact cause and how badly the tissue that lines the esophagus is damaged. Without treatment, esophagitis can damage this lining. The esophagus may start to have trouble moving food and liquid from the mouth to the stomach. Esophagitis also can lead to other serious health issues. These include scarring or narrowing of the esophagus, unhealthy weight loss, and dehydration.
Symptoms
Common symptoms of esophagitis include:
- Trouble swallowing.
- Painful swallowing.
- Swallowed food becoming stuck in the esophagus, also known as food impaction.
- Burning pain in the chest called heartburn. It's common to feel this pain behind the breastbone while eating.
- Stomach acid that backs up into the esophagus, also called acid reflux.
Babies and some children with esophagitis are too young to explain their discomfort or pain. Their symptoms can include:
- Feeding troubles, such as getting easily upset, arching of the back and not wanting to eat.
- Failure to thrive.
- Chest or belly pain in older children.
When to see a doctor
Most symptoms of esophagitis can be caused by a few different conditions that affect the digestive system. See your healthcare professional if the symptoms:
- Last more than a few days.
- Don't get better after using medicines called antacids that are available without a prescription.
- Are bad enough to make it hard for you to eat or cause you to lose weight.
- Happen along with flu symptoms such as headache, fever and muscle aches.
Get emergency care if you:
- Have pain in your chest that lasts more than a few minutes.
- Think you have food stuck in your esophagus.
- Have a history of heart disease and feel chest pain.
- Feel pain in your mouth or throat when you eat.
- Have shortness of breath or chest pain that happens soon after eating.
- Vomit large amounts, often have forceful vomiting or have trouble breathing after vomiting.
- Notice that your vomit is yellow or green, looks like coffee grounds, or has blood in it.
Causes
Healthcare professionals tend to label esophagitis by the condition that causes it. Sometimes, esophagitis may have more than one cause. Some of the most common types include the following:
Reflux esophagitis
A valve called the lower esophageal sphincter usually keeps stomach acid out of the esophagus. But sometimes this valve doesn't close properly. Or it opens when it shouldn't. In some people, the upper part of the stomach bulges through the large muscle that separates the stomach and the chest. This is known as a hiatal hernia. It also can cause stomach acid to back up into the esophagus.
Gastroesophageal reflux disease (GERD) is a condition in which this backflow of acid is a frequent or ongoing problem. GERD can lead to ongoing swelling and tissue damage in the esophagus.
Eosinophilic esophagitis
Eosinophilic esophagitis
Eosinophilic esophagitis
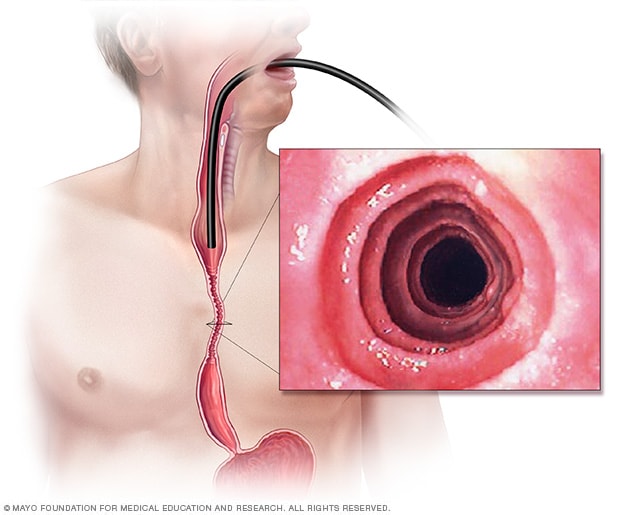
Esophagitis is swelling and irritation, called inflammation, of the tissues that line the esophagus. A long, flexible tube that’s tipped with a camera, called an endoscope, can be used to see inside the esophagus. This endoscopic image of eosinophilic esophagitis shows irritated rings of irregular tissue that stem from ongoing inflammation. These are known as esophageal rings.
Eosinophils (e-o-SIN-o-fils) are white blood cells that play a key role in allergic reactions. Eosinophilic esophagitis can happen if lots of these white blood cells build up in the esophagus. This most likely happens in response to a substance that causes an allergy, acid reflux or both.
Certain foods may trigger this type of esophagitis, including:
- Milk.
- Eggs.
- Wheat.
- Soy.
- Peanuts.
- Seafood.
Typical allergy testing often is not able to spot these foods as being triggers.
People with eosinophilic esophagitis may have other allergies that aren't caused by food. For example, sometimes allergens in the air, such as pollen, may be the cause. One common symptom of eosinophilic esophagitis is food getting stuck in the esophagus after swallowing. This is called food impaction. Another common symptom is trouble swallowing, also called dysphagia.
Lymphocytic esophagitis
Lymphocytic esophagitis (LE) isn't a common condition of the esophagus. With LE, a higher than typical number of white blood cells called lymphocytes build up in the lining of the esophagus. LE may be related to eosinophilic esophagitis or to GERD.
Medicine-induced esophagitis
Also called drug-induced esophagitis, this type happens when some medicines taken by mouth cause tissue damage in the esophagus. The damage happens if the medicines stay in contact with the lining of the esophagus for too long. For example, you might swallow a pill with little or no water. If you do that, the pill itself or residue from the pill may stay in the esophagus. Medicines that have been linked to esophagitis include:
- Pain-relieving medicines such as aspirin, ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
- Antibiotics such as tetracycline and doxycycline.
- Medicine called potassium chloride that is used to treat low levels of the mineral potassium.
- Medicines called bisphosphonates that treat bone conditions such as osteoporosis. These medicines include alendronate (Binosto, Fosamax).
- A treatment for heart conditions called quinidine.
Infectious esophagitis
An infection in tissues of the esophagus may cause esophagitis. The infection could be due to bacteria, viruses or funguses. Infectious esophagitis is fairly rare. It happens most often in people with weakened immune systems, such as people with HIV/AIDS or cancer.
A fungus usually present in the mouth called Candida albicans is a common cause of infectious esophagitis. This type of fungal infection often is linked with a weakened immune system, diabetes, cancer, or use of steroid or antibiotic medicines.
Risk factors
Risk factors for esophagitis vary depending on the cause of the condition.
Reflux esophagitis
Factors that raise the risk of gastroesophageal reflux disease (GERD) also are factors in reflux esophagitis. These risk factors include the following:
- Eating right before going to bed.
- Eating meals that are too large and fatty.
- Smoking.
- Gaining extra weight, including from pregnancy.
Foods that can make symptoms of GERD or reflux esophagitis worse include:
- Caffeine.
- Alcohol.
- Fatty foods.
- Chocolate.
- Peppermint.
Eosinophilic esophagitis
Risk factors for this allergy-related esophagitis may include:
- A history of certain allergic reactions. These include asthma, atopic dermatitis and allergic rhinitis, also known as hay fever.
- A family history of eosinophilic esophagitis.
Medicine-induced esophagitis
Risk factors for this type of esophagitis often are linked with issues that prevent quick and complete passage of a pill into the stomach. These factors include:
- Swallowing a pill with little or no water.
- Taking medicines while lying down.
- Taking medicines right before sleep. This risk factor likely is due in part to less saliva being made and less swallowing happening during sleep.
- Being older in age. This may be a factor because of age-related changes to the muscles of the esophagus or to glands making less saliva.
- Taking large or oddly shaped pills.
Infectious esophagitis
Risk factors for infectious esophagitis often relate to medicines such as steroids or antibiotics. People with diabetes also have a higher risk of esophagitis caused by a fungal candida infection in particular.
Other causes of infectious esophagitis may relate to poor immune system function. This may be due to an immune system condition, such as HIV/AIDS, or certain cancers. Also, certain cancer treatments may raise the risk of infectious esophagitis. So might medicines called immunosuppressants that block immune system reactions to transplanted organs.
Complications
Without treatment, esophagitis can lead to changes in the structure of the esophagus. Complications can include:
- Scarring or narrowing of the esophagus, known as a stricture.
- Tearing of the lining of the esophagus. This can be due to retching or to healthcare professionals passing medical tools through an inflamed esophagus during endoscopy. Endoscopy is a way for healthcare professionals to check the digestive system.
- A condition called Barrett esophagus in which the cells lining the esophagus are damaged from acid reflux. This raises the risk of cancer that starts in the esophagus, also called esophageal cancer.
Oct. 29, 2024