Overview
Emphysema
Emphysema
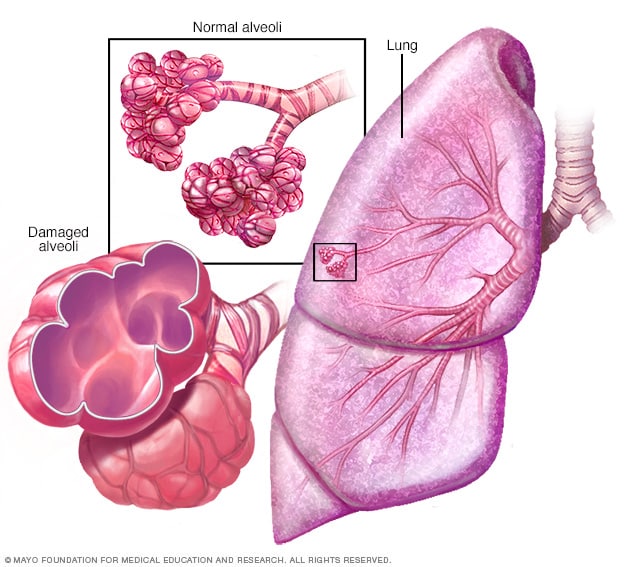
In emphysema, the inner walls of the lungs' air sacs called alveoli are damaged, causing them to eventually rupture. This creates one larger air space instead of many small ones and reduces the surface area available for gas exchange.
Emphysema is a long-term lung condition that causes shortness of breath. Over time, the condition damages the thin walls of the air sacs in the lungs called alveoli. In healthy lungs, these sacs stretch and fill with air when you breathe in. The elastic sacs help the air leave when you breathe out. But when the air sacs are damaged in emphysema, it's hard to move air out of your lungs. This doesn't leave room for fresh, oxygen-rich air to enter your lungs.
Symptoms of emphysema include trouble breathing, especially with activity, and a wheezing sound when breathing out. How severe the condition is can vary.
Smoking is the leading cause of emphysema. Treatment can help with symptoms and may slow how fast the condition gets worse. But it can't reverse the damage.
Products & Services
Symptoms
You can have emphysema for many years without noticing any symptoms. They usually begin gradually and include:
- Shortness of breath, especially with physical activity. This is the main symptom of emphysema.
- Wheezing, whistling or squeaking sound when you breathe out.
- Coughing.
- Chest tightness or heaviness.
- Feeling very tired.
- Weight loss and ankle swelling that may happen as the condition gets worse over time.
You may start avoiding activities that cause you to be short of breath, so the symptoms don't become a problem until they keep you from doing daily tasks. Emphysema eventually causes trouble breathing even while you're resting.
Emphysema is one of the two common types of chronic obstructive pulmonary disease (COPD). The other common type is chronic bronchitis. In chronic bronchitis, the lining of the tubes that carry air to your lungs, called bronchial tubes, become irritated and swollen. This inflammation limits the space for air to move in and out of the lungs and makes extra mucus that blocks the airways. Emphysema and chronic bronchitis often occur together, so the general term COPD may be used.
Exacerbations
Even with ongoing treatment, you may have times when symptoms become worse for days or weeks. This is called an acute exacerbation (eg-zas-er-bay-shun). It may lead to lung failure if you don't receive prompt treatment.
Exacerbations may be caused by a respiratory infection, air pollution or other things that trigger inflammation. Whatever the cause, it's important to get medical help promptly if you notice an ongoing worsening cough or extra mucus, or if you have a harder time breathing.
When to see a doctor
See your healthcare professional if you've had shortness of breath you can't explain for several months, especially if it's getting worse or if it's keeping you from doing your daily activities. Don't ignore it or tell yourself it's because you're aging or out of shape.
Go to the emergency department at a hospital if:
- You're having a hard time catching your breath or talking.
- Your lips or fingernails turn blue or gray with physical activity.
- Others notice that you're not mentally alert.
Causes
Emphysema results from long-term exposure to airborne irritants, including:
- Smoking cigarettes, which is the most common cause.
- Chemical fumes, especially in the workplace.
- Vapors and dusts, especially in the workplace.
Rarely, emphysema results from a gene change passed down in families. This gene change causes low levels of a protein called alpha-1-antitrypsin (AAT). AAT is made in the liver and is passed into the bloodstream to help protect the lungs from damage caused by smoke, fumes and dust. Low levels of AAT, a condition called alpha-1-antitrypsin deficiency, can cause liver damage, lung conditions such as emphysema or both. With AAT deficiency, there is usually a family history of emphysema, and symptoms begin at a younger age.
Risk factors
Lung damage in emphysema develops gradually. In most people with the condition, symptoms start after age 40.
Factors that increase your risk of developing emphysema include:
- Smoking. Smoking cigarettes or having smoked in the past is the biggest risk factor for emphysema. But people who smoke cigars, pipes or marijuana also are at risk. The risk for all types of smokers increases with the number of years of smoking and the amount of tobacco smoked.
- Being around secondhand smoke. Secondhand smoke is smoke that you breathe in from someone else's cigarette, pipe or cigar. Being around secondhand smoke raises your risk of emphysema.
- Job exposure to fumes, vapors or dust. If you breathe in fumes or vapors from certain chemicals or dust from grain, cotton, wood or mining products, you're more likely to develop emphysema. This risk is even greater if you also smoke.
- Exposure to indoor and outdoor pollution. Breathing indoor pollutants, such as fumes from heating fuel, as well as outdoor pollutants, such as smog or car exhaust, increases your risk of emphysema.
- Genetics. The uncommon condition called AAT deficiency raises the risk of emphysema. Other genetic factors may make certain smokers more likely to get emphysema.
Complications
People who have emphysema are more likely to develop:
- High blood pressure in lung arteries. Emphysema may cause high blood pressure in the arteries that bring blood to the lungs. This serious condition is called pulmonary hypertension. Pulmonary hypertension can cause the right side of the heart to expand and weaken, a condition called cor pulmonale.
- Other heart problems. For reasons that aren't fully understood, emphysema can raise your risk of heart disease, including heart attack.
- Large air spaces in the lungs. Large air spaces called bullae form in the lungs when the inner walls of the alveoli are destroyed. This leaves one very large air sac instead of a cluster of many smaller ones. These bullae can become very large, even as large as half the lung. The bullae lessen the space available for the lung to expand. Also, giant bullae can increase the risk of a collapsed lung.
- Collapsed lung. A collapsed lung called pneumothorax can be life-threatening in people who have severe emphysema because their lungs are already damaged. This is not common but it's serious when it happens.
- Lung cancer. People with emphysema have a higher risk of getting lung cancer. Smoking raises this risk even more.
- Anxiety and depression. Problems breathing can keep you from doing activities that you enjoy. And having a serious medical condition such as emphysema can sometimes cause anxiety and depression.
Prevention
To prevent emphysema or to keep symptoms from getting worse:
- Don't smoke. Talk to your healthcare professional about options for quitting.
- Stay away from secondhand smoke.
- Wear a special mask or use other measures to protect your lungs if you work with chemical fumes, vapors or dust.
- Avoid exposure to secondhand smoke and air pollution when possible.
Nov. 19, 2024