Diagnosis
Breast calcifications

Breast calcifications
Calcifications are small buildups of calcium, called calcium deposits, in the breast. They show up as white spots on a mammogram. Large, round or well-defined calcifications (shown left) are more likely to not be cancer, also called benign. Tight clusters of tiny, fine, irregularly shaped calcifications (shown right) may mean cancer.
Stereotactic breast biopsy
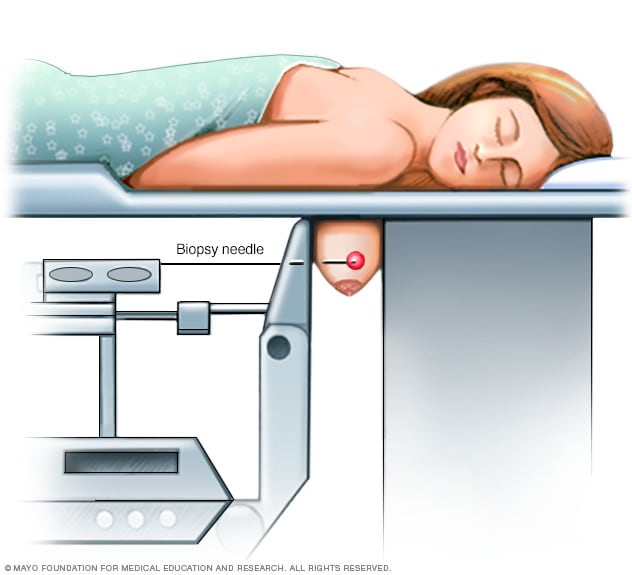
Stereotactic breast biopsy
During a stereotactic breast biopsy, the breast is firmly compressed between two plates. Breast X-rays, called mammograms, are used to produce stereo images. Stereo images are images of the same area from different angles. They help to determine the exact location for the biopsy. A sample of breast tissue in the area of concern is then removed with a needle.
Core needle biopsy
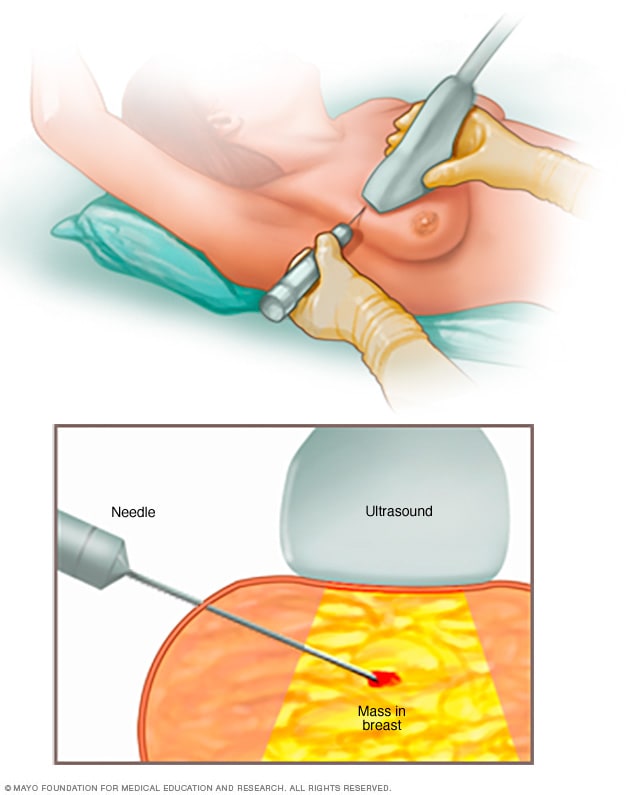
Core needle biopsy
A core needle biopsy uses a long, hollow tube to obtain a sample of tissue. Here, a biopsy of a suspicious breast lump is being done. The sample is sent to a lab for testing by doctors called pathologists. They specialize in examining blood and body tissue.
Ductal carcinoma in situ, also called DCIS, is most often discovered during a mammogram used to screen for breast cancer. A mammogram is an X-ray of the breast tissue. If your mammogram shows something concerning, you will likely have additional breast imaging and a biopsy.
Mammogram
If an area of concern was found during a screening mammogram, you may then have a diagnostic mammogram. A diagnostic mammogram takes views at higher magnification from more angles than a mammogram used for screening. This examination evaluates both breasts.
A diagnostic mammogram gives your healthcare team a closer look at any calcium deposits detected in the breast tissue. Calcium deposits, also called calcifications, can sometimes be cancerous.
If the area of concern needs further evaluation, the next step may be an ultrasound and a breast biopsy.
Breast ultrasound
Ultrasound uses sound waves to make images of structures inside the body. A breast ultrasound may give your healthcare team more information about an area of concern. The healthcare team uses this information to decide what tests you might need next.
Removing breast tissue samples for testing
A biopsy is a procedure to remove a sample of tissue for testing in a lab. For DCIS, a healthcare professional removes the sample of breast tissue using a special needle. The needle used is a hollow tube. The healthcare professional puts the needle through the skin on the breast and into the area of concern. The health professional draws out some of the breast tissue. This procedure is called a core needle biopsy.
Often the healthcare professional uses an imaging test to help guide the needle to the right spot. A biopsy that uses ultrasound is called an ultrasound-guided breast biopsy. If it uses X-rays, it's called a stereotactic breast biopsy. The tissue samples are sent to a lab for testing.
In a lab, a doctor who specializes in analyzing blood and body tissue looks at the tissue samples. This doctor is called a pathologist. The pathologist can tell whether cancer cells are present and if so, how aggressive those cells appear to be.
More Information
Treatment
Lumpectomy
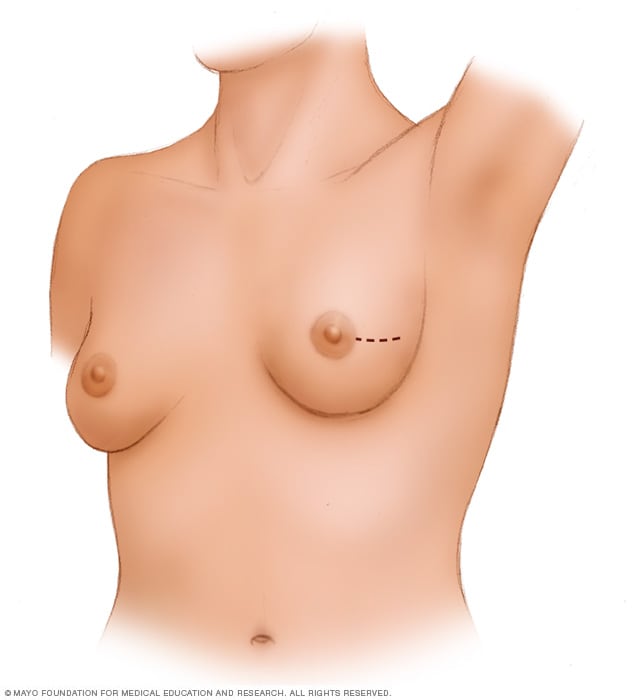
Lumpectomy
A lumpectomy involves removing the cancer and some of the healthy tissue that surrounds it. This illustration shows one possible incision that can be used for this procedure, though your surgeon will determine the approach that's best for your particular situation.
Radiation therapy
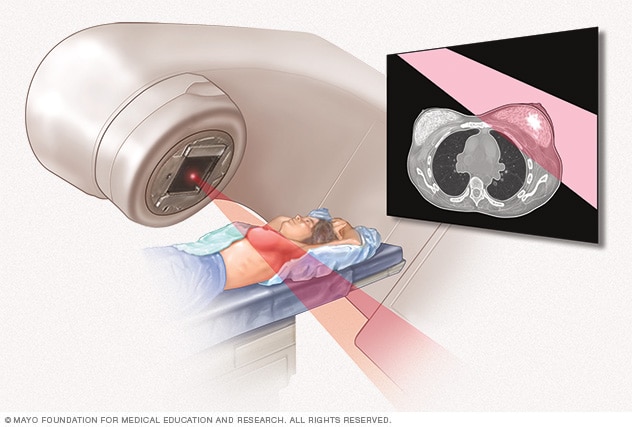
Radiation therapy
External beam radiation uses high-powered beams of energy to kill cancer cells. Beams of radiation are precisely aimed at the cancer using a machine that moves around your body.
Ductal carcinoma in situ can often be cured. Treatment for this very early form of breast cancer often involves surgery to remove the cancer. Ductal carcinoma in situ, also called DCIS, also may be treated with radiation therapy and medicines.
DCIS treatment has a high likelihood of success. In most instances, the cancer is removed and has a low chance of coming back after treatment.
In most people, treatment options for DCIS include:
- Breast-conserving surgery, called a lumpectomy, and radiation therapy.
- Breast-removing surgery, called a mastectomy.
In some people, treatment options may include:
- Lumpectomy only.
- Lumpectomy and hormone therapy.
Surgery
If you're diagnosed with DCIS, one of the first decisions you'll have to make is whether to treat the condition with lumpectomy or mastectomy.
-
Lumpectomy. A lumpectomy is surgery to remove the breast cancer and some of the healthy tissue around it. The rest of the breast tissue isn't removed. Other names for this surgery are breast-conserving surgery and wide local excision. Most people who have a lumpectomy also have radiation therapy.
Research suggests that there is a slightly higher risk of the cancer coming back after lumpectomy compared to mastectomy. However, survival rates between the two treatment approaches are very similar.
If you have other serious health conditions, you might consider other options, such as lumpectomy plus hormone therapy, lumpectomy alone or no treatment.
- Mastectomy. A mastectomy is surgery to remove all breast tissue from a breast. Breast reconstruction to restore the appearance of the breast can be done at the same time or in a later procedure, if you desire.
Lumpectomy is a good option for most people with DCIS. But mastectomy may be recommended if:
- You have a large area of DCIS. If the area is large relative to the size of your breast, a lumpectomy may not produce acceptable cosmetic results.
- There's more than one area of DCIS. When there are multiple areas of DCIS, it is called multifocal or multicentric disease. It's difficult to remove multiple areas of DCIS with a lumpectomy. This is especially true if DCIS is found in different parts of the breast.
- Biopsy results show cancer cells at or near the edge of the tissue sample. There may be more DCIS than originally thought. This means that a lumpectomy might not be enough to remove all areas of DCIS. A mastectomy could be needed to remove all of the breast tissue.
- You're not a candidate for radiation therapy. Radiation is usually given after a lumpectomy. Radiation might not be an option if you're in the first trimester of pregnancy or if you've received radiation to your chest or breast in the past. It also might not be recommended if you have a condition that makes you more sensitive to radiation side effects, such as systemic lupus erythematosus.
- You prefer to have a mastectomy. For instance, you might not want a lumpectomy if you don't want to have radiation therapy.
Because DCIS is noninvasive, surgery typically doesn't involve the removal of lymph nodes from under your arm. The chance of finding cancer in the lymph nodes is extremely small.
If your healthcare team thinks the cancer cells may have spread outside the breast duct or if you are having a mastectomy, then some lymph nodes may be removed as part of the surgery.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources.
For DCIS treatment, the radiation is often external beam radiation. During this type of radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body. Less often, the radiation can be placed inside the body. This type of radiation is called brachytherapy.
Radiation therapy is often used after lumpectomy to reduce the chance that DCIS will come back or that it will progress to invasive cancer. But it might not be necessary if you have only a small area of DCIS that is considered slow-growing and was completely removed during surgery.
Hormone therapy
Hormone therapy, also called endocrine therapy, uses medicines to block certain hormones in the body. It's a treatment for breast cancers that are sensitive to the hormones estrogen and progesterone. Healthcare professionals call these cancers estrogen receptor positive and progesterone receptor positive. Cancers that are sensitive to hormones use the hormones as fuel for their growth. Blocking the hormones can cause the cancer cells to shrink or die.
For DCIS, hormone therapy is typically used after surgery or radiation. It lowers the risk that the cancer will come back. It also reduces the risk of developing another breast cancer.
Treatments that can be used in hormone therapy include:
- Medicines that block hormones from attaching to cancer cells. These medicines are called selective estrogen receptor modulators. Examples include tamoxifen and raloxifene (Evista).
- Medicines that stop the body from making estrogen after menopause. These medicines are called aromatase inhibitors. Examples include anastrozole (Arimidex), exemestane (Aromasin) and letrozole (Femara).
Discuss the benefits and risks of hormone therapy with your healthcare team.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Alternative medicine
No alternative medicine treatments have been found to cure ductal carcinoma in situ, also called DCIS. But complementary and alternative medicine therapies may help you cope with side effects of treatment.
Combined with your healthcare team's recommendations, complementary and alternative medicine treatments may provide some comfort. Examples include:
- Art therapy.
- Exercise.
- Meditation.
- Music therapy.
- Relaxation exercises.
- Spirituality.
Coping and support
A diagnosis of ductal carcinoma in situ, also called DCIS, can feel overwhelming. To cope with your diagnosis, it may be helpful to:
Learn enough about DCIS to make decisions about your care
Ask your healthcare team questions about your diagnosis and your pathology results. Use this information to research your treatment options.
Knowing more about your cancer and your options may help you feel more confident when making treatment decisions. Still, some people don't want to know the details of their cancer. If this is how you feel, let your care team know that too.
Find someone to talk with about your feelings
Find a friend or family member who is a good listener. Or talk with a clergy member or counselor. Ask your healthcare team for a referral to a counselor or other professional who works with people who have cancer.
Keep your friends and family close
Your friends and family can provide a crucial support network for you during your cancer treatment.
As you begin telling people about your breast cancer diagnosis, you'll likely get many offers for help. Think ahead about things you may want help with. Examples include listening when you want to talk or helping you with preparing meals.
Preparing for your appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you. If an exam or imaging test shows that you might have ductal carcinoma in situ, also called DCIS, your healthcare team will likely refer you to a specialist.
Specialists who care for people with DCIS include:
- Breast health specialists.
- Breast surgeons.
- Doctors who specialize in diagnostic tests, such as mammograms, called radiologists.
- Doctors who specialize in treating cancer, called oncologists.
- Doctors who treat cancer with radiation, called radiation oncologists.
- Genetic counselors.
- Plastic surgeons.
Here's some information to help you get ready for your appointment.
What you can do
- Write down your medical history, including any benign breast conditions with which you've been diagnosed. Also mention any radiation therapy you may have received, even years ago.
- Write down your family history of cancer. Note any family members who have had cancer. Note how each member is related to you, the type of cancer, the age at diagnosis and whether each person survived.
- Make a list of all medicines, vitamins or supplements that you're taking. If you're currently taking or have previously taken hormone replacement therapy, tell your healthcare provider.
- Consider taking a family member or friend along. Sometimes it can be difficult to absorb all the information provided during an appointment. Someone who comes with you may remember something that you missed or forgot.
- Write down questions to ask your healthcare professional.
Questions to ask your doctor
Your time with your healthcare professional is limited. Prepare a list of questions so that you can make the most of your time together. List your questions from most important to least important in case time runs out. For breast cancer, some basic questions to ask include:
- Do I have breast cancer?
- What tests do I need to determine the type and stage of cancer?
- What treatment approach do you recommend?
- What are the possible side effects or complications of this treatment?
- In general, how effective is this treatment?
- Am I a candidate for tamoxifen?
- Am I at risk of this condition recurring?
- Am I at risk of developing invasive breast cancer?
- How will you treat DCIS if it returns?
- How often will I need follow-up visits after I finish treatment?
- What lifestyle changes can help reduce my risk of a DCIS recurrence?
- Do I need a second opinion?
- Should I see a genetic counselor?
In addition to the questions that you've prepared, don't hesitate to ask other questions you think of during your appointment.
What to expect from your doctor
Be prepared to answer some questions about your symptoms and your health, such as:
- Have you gone through menopause?
- Are you using or have you used any medicines or supplements to relieve the symptoms of menopause?
- Have you had other breast biopsies or operations?
- Have you been diagnosed with any breast conditions, including noncancerous conditions?
- Have you been diagnosed with any other medical conditions?
- Do you have any family history of breast cancer?
- Have you or your female blood relatives ever been tested for BRCA gene mutations?
- Have you ever had radiation therapy?
- What is your typical daily diet, including alcohol intake?
- Are you physically active?
July 19, 2024
- Niederhuber JE, et al., eds. Cancer of the breast. In: Abeloff's Clinical Oncology. 6th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed March 1, 2024.
- Townsend CM Jr, et al. Diseases of the breast. In: Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 21st ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed March 1, 2024.
- Breast cancer. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1419. Accessed March 1, 2024.
- Abraham J, et al., eds. Breast cancer. In: The Bethesda Handbook of Clinical Oncology. 6th ed. Kindle edition. Wolters Kluwer; 2023. Accessed March 1, 2024.
- Collins LC, et al. Breast ductal carcinoma in situ: Epidemiology, clinical manifestations, and diagnosis. https://www.uptodate.com/contents/search. Accessed March 1, 2024.
- Distress management. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1431. Accessed March 1, 2024.
- Record SM, et al. How to navigate the treatment spectrum from multimodality therapy to observation alone for ductal carcinoma in situ. Surgical Oncology Clinics of North America. 2023; doi:10.1016/j.soc.2023.05.011.
- Breast cancer prevention (PDQ) – Patient version. National Cancer Institute. https://www.cancer.gov/types/breast/patient/breast-prevention-pdq. Accessed March 1, 2024.
Related
Associated Procedures
Products & Services
Ductal carcinoma in situ (DCIS)