Overview
What is cystic fibrosis? A Mayo Clinic expert explains
Learn more from pulmonologist Sarah Chalmers, M.D.
Hello. I'm Dr. Sarah Chalmers, a pulmonologist at Mayo Clinic. In this video, we'll cover the basics of cystic fibrosis. What is it? Who gets it? The symptoms, diagnosis and treatment. Whether you're looking for answers for yourself or someone you love, we're here to give you the best information available. Cystic fibrosis is a disorder that damages your lungs, digestive tract and other organs. It's an inherited disease caused by a defective gene that can be passed from generation to generation. Cystic fibrosis affects the cells that produce mucus, sweat and digestive juices. These secreted fluids are normally thin and slippery. But in people with CF, they're thick and sticky. Instead of acting as lubricants, these secretions plug up the tubes, ducts and airways in your body. Although there is no cure for cystic fibrosis, people with this condition are generally able to live normal lives. There are many tools and techniques doctors use to help manage this complicated condition and with improvement in screening and treatments, life expectancy for those with cystic fibrosis is better than ever before.
Simply put, cystic fibrosis is a gene defect. A defect to this gene changes how a salt moves in and out of cells, resulting in thick, sticky mucus in the respiratory, digestive and reproductive systems. It's an inherited condition. A child needs to inherit one copy of the mutated gene from each parent to develop cystic fibrosis. If they only inherit one copy from one parent, they won't develop it. However, they will be a carrier of that mutated gene, so they could pass it along to their own children in the future. Because CF is an inherited disorder, family history determines your risk. Although it can occur in all races, cystic fibrosis is most common in white people of North European ancestry.
There are two kinds of symptoms associated with cystic fibrosis. The first are respiratory symptoms. Thick, sticky mucus can clog the tubes that carry air in and out of your lungs. This can trigger a persistent cough that produces thick mucus, wheezing, exercise intolerance, repeated lung infections, and inflamed nasal passages or a stuffy nose or recurrent sinusitis. The second type of symptoms are digestive. That same thick mucus that can clog your airways can also bog tubes that carry enzymes from your pancreas to your small intestine. This can result in foul-smelling or greasy stools, poor weight gain and growth, intestinal blockage, or chronic and severe constipation, which may include frequent straining while trying to pass stool. If you or your child show symptoms of cystic fibrosis or if someone in your family has CF, talk with your doctor about testing for the disease.
Since this disease is an inherited condition, reviewing your family history is important. Genetic testing may be done to see if you carry the mutated gene that triggers cystic fibrosis. A sweat test may also be conducted. CF causes higher than normal levels of salt in your sweat. Doctors will examine the levels of salt in your sweat to confirm a diagnosis.
Because this condition is passed from parent to children, newborn screening is routinely done in every state in the U.S. Early diagnosis of CF means that treatments can begin immediately. Unfortunately, there is no cure for cystic fibrosis, but proper treatment can ease your symptoms, reduce complications, and improve your quality of life. Doctors may decide that certain medications are necessary. These could include antibiotics to treat and prevent lung infections, anti-inflammatories to lessen the swelling in your airways, or mucus-thinning drugs to help expel mucus and improve lung function. Medications can also help improve digestive function. From stool softeners to enzymes, to acid-reducing drugs. Some medications can even target the gene defect that causes cystic fibrosis, aiding the faulty proteins to improve lung function and reduce salt in your sweat. Outside of medications, airway clearance techniques, also called chest physical therapy, can relieve mucus obstruction and help to reduce infection and inflammation in the airways. These techniques loosen the thick mucus in the lungs, making it easier to cough up. In some cases, doctors turn to surgery to help alleviate conditions that can arise from cystic fibrosis. For instance, nasal and sinus surgery to help you breathe, or bowel surgery to help improve digestive function. In life-threatening instances, lung transplant and liver transplant had been performed. Managing cystic fibrosis can be very complex. So consider getting treatment at a center with medical professionals trained in the disorder to evaluate and treat your condition. You can even ask your physician about clinical trials. New treatments, interventions and tests are constantly under development to help prevent, detect, and treat this disease.
Learning you or someone you know has cystic fibrosis can be incredibly challenging. It's okay to feel depressed, anxious, angry, or afraid. In time, you'll find ways to cope, find support and talk to others who are going through it too. Look to your friends and family to help manage stress and reduce anxiety. Seek professional help. Remember, physical conditions come with an emotional and mental burden. And take the time to learn about cystic fibrosis. It's a complicated, severe disorder. So don't hesitate to talk to your medical team about your questions or concerns. With the knowledge and treatment available to doctors today, life with cystic fibrosis is better than ever before. If you'd like to learn even more about cystic fibrosis, watch our other related videos or visit mayoclinic.org. We wish you well.
Cystic fibrosis (CF) is a condition passed down in families that causes damage to the lungs, digestive system and other organs in the body.
CF affects the cells that make mucus, sweat and digestive juices. These fluids, also called secretions, are usually thin and slippery to protect the body's internal tubes and ducts and make them smooth pathways. But in people with CF, a changed gene causes the secretions to become sticky and thick. The secretions plug up pathways, especially in the lungs and pancreas.
CF gets worse over time and needs daily care, but people with CF usually can attend school and work. They often have a better quality of life than people with CF had in past decades. Better screening and treatments mean that people with CF now may live into their mid- to late 50s or longer, and some are being diagnosed later in life.
Cystic fibrosis
Cystic fibrosis
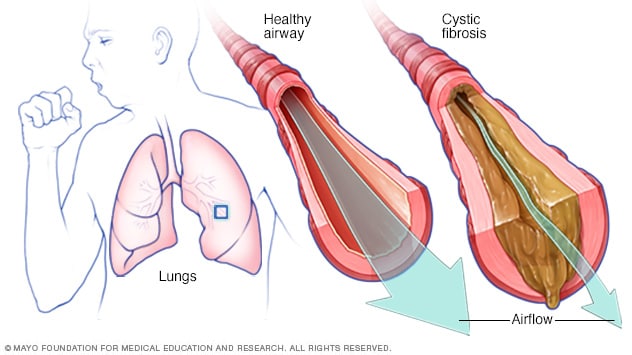
In cystic fibrosis, the airways fill with thick, sticky mucus, making it difficult to breathe. The thick mucus is also an ideal breeding ground for bacteria and fungi.
Products & Services
Symptoms
In the U.S., because of newborn screening, cystic fibrosis can be diagnosed within the first month of life, before symptoms develop. But people born before newborn screening became available may not be diagnosed until the symptoms of CF show up.
CF symptoms vary, depending on which organs are affected and how severe the condition is. Even in the same person, symptoms may worsen or get better at different times. Some people may not have symptoms until their teenage years or adulthood.
People who are not diagnosed until adulthood usually have milder symptoms and are more likely to have symptoms that aren't typical. These may include repeated bouts of an inflamed pancreas called pancreatitis, infertility and repeated bouts of pneumonia.
People with CF have a higher than usual level of salt in their sweat. Parents often can taste the salt when they kiss their children. Most of the other symptoms of CF affect the respiratory system and digestive system.
Respiratory symptoms
In cystic fibrosis, the lungs are most commonly affected. The thick and sticky mucus that happens with CF clogs the tubes that carry air in and out of the lungs. This can cause symptoms such as:
- A cough that won't go away and brings up thick mucus.
- A squeaking sound when breathing called wheezing.
- Limited ability to do physical activity before tiring.
- Repeated lung infections.
- Irritated and swollen nasal passages or a stuffy nose.
- Repeated sinus infections.
Digestive symptoms
The thick mucus caused by cystic fibrosis can block tubes that carry digestive enzymes from the pancreas to the small intestine. Without these digestive enzymes, the intestines can't completely take in and use the nutrients in food. The result is often:
- Foul-smelling, greasy stools.
- Poor weight gain and growth.
- Blocked intestines, which is more likely to happen in newborns.
- Ongoing or severe constipation. Straining often while trying to pass stool can cause part of the rectum to stick out of the anus. This is called a rectal prolapse.
When to see a doctor
If you or your child has symptoms of cystic fibrosis — or if someone in your family has CF — talk with your healthcare professional about testing for the condition. Make an appointment with a doctor who has skills and experience in treating CF.
CF requires regular follow-up with your healthcare professional, at least every three months. Call your healthcare professional if you have new or worsening symptoms, such as more mucus than usual or a change in the mucus color, lack of energy, weight loss, or severe constipation.
Get medical care right away if you're coughing up blood, have chest pain or trouble breathing, or have severe stomach pain and bloating.
Call 911 or your local emergency number or go to the emergency department at a hospital if:
- You're having a hard time catching your breath or talking.
- Your lips or fingernails turn blue or gray.
- Others notice that you're not mentally alert.
Causes
Autosomal recessive inheritance pattern

Autosomal recessive inheritance pattern
To have an autosomal recessive disorder, you inherit two changed genes, sometimes called mutations. You get one from each parent. Their health is rarely affected because they have only one changed gene. Two carriers have a 25% chance of having an unaffected child with two unaffected genes. They have a 50% chance of having an unaffected child who also is a carrier. They have a 25% chance of having an affected child with two changed genes.
In cystic fibrosis, a change in a gene causes problems with the protein that controls the movement of salt and water in and out of cells. This gene is the cystic fibrosis transmembrane conductance regulator (CFTR) gene. It affects the cells that make mucus, sweat and digestive juices. When the CFTR protein doesn't work as it should, the result is thick, sticky mucus in the respiratory, digestive and reproductive systems, as well as extra salt in sweat.
Changes in the CFTR gene that cause CF are divided into several different groups based on the problems they cause. Different groups of gene changes affect how much CFTR protein is made and how well it works.
To have cystic fibrosis, children must get one copy of the changed CFTR gene from each parent. If children get only one copy, they won't develop CF. But they will be carriers and could pass the changed gene to their own children. People who are carriers may have no symptoms of CF or a few mild symptoms.
Risk factors
Because cystic fibrosis is a condition passed down in families, family history is a risk factor.
CF occurs in all races, but it's most common in white people of Northern European ancestry. Because it's less common in people who are Black, Hispanic, Middle Eastern, Native American or Asian, this might lead to a much later diagnosis.
A late diagnosis may cause worse health issues. Early and effective treatment can improve your quality of life, prevent complications and help you live longer. If you're a person of color and have symptoms that could be CF, talk to your healthcare professional so that you can get tested for CF.
Complications
Complications of cystic fibrosis can affect the respiratory, digestive and reproductive systems, as well as other organs.
Respiratory system complications
- Damaged airways. Cystic fibrosis is one of the leading causes of damaged airways, a long-term lung condition called bronchiectasis. Bronchiectasis results in widening and scarring of the airways. This makes it harder to move air in and out of the lungs and clear mucus from the airways.
- Ongoing infections. Thick mucus in the lungs and sinuses makes a place for bacteria and fungi to live and grow. Sinus infections, bronchitis or pneumonia are common and may happen repeatedly. Infections with bacteria that don't respond to antibiotics and are difficult to treat is common too.
- Growths in the nose. Because the lining inside the nose is irritated and swollen, it can develop soft, fleshy growths called nasal polyps.
- Coughing up blood. Bronchiectasis can occur next to blood vessels in the lungs. The combination of airway damage and infection can result in coughing up blood. Often this is only a small amount of blood, but rarely it can be life-threatening.
- Collapsed lung. Also called pneumothorax, this condition happens when air leaks into the space that separates the lungs from the chest wall. This causes part or all of a lung to collapse. Collapsed lung is more common in adults with CF. Collapsed lung can cause sudden chest pain and trouble breathing. People often have a bubbling feeling in the chest.
- Respiratory failure. Over time, CF can damage lung tissue so badly that it no longer works. Lung function usually worsens slowly over time and can become life-threatening. Respiratory failure is the most common cause of death with CF.
- Bouts of worsening symptoms. People with CF may experience times when respiratory symptoms are worse than usual. These are called exacerbations (eg-zas-er-bay-shuns). Symptoms may include coughing with more mucus than usual and trouble breathing. Low energy and weight loss also are common during exacerbations. Exacerbations are treated with antibiotics. Sometimes treatment can be given at home, but a stay in the hospital may be needed.
Digestive system complications
- Poor nutrition. Thick mucus can block the tubes that carry digestive enzymes from the pancreas to the intestines. Without these enzymes, the body can't take in and use protein, fats or fat-soluble vitamins and can't get enough nutrients. This can result in delayed growth and weight loss. An inflamed pancreas, a condition called pancreatitis, is common.
- Diabetes. The pancreas makes insulin, which the body needs to use sugar. Cystic fibrosis raises the risk of diabetes. About 20% of teenagers and up to 50% of adults with CF develop diabetes.
- Liver disease. The tube that carries bile from the liver and gallbladder to the small intestine may become blocked and inflamed. This can lead to liver problems, such as jaundice, fatty liver disease and cirrhosis, and sometimes gallstones.
- Intestinal obstruction. Intestinal blockage can happen to people with CF at all ages. Sometimes, a condition in which a section of the intestine slides inside another nearby section of the intestine, like a collapsible telescope, also can happen.
- Distal intestinal obstruction syndrome (DIOS). DIOS is partial or complete blockage where the small intestine meets the large intestine. DIOS requires treatment right away.
Reproductive system complications
- Infertility in men. Almost all men with cystic fibrosis are not fertile. The tube that connects the testicles and prostate gland, called the vas deferens, is either blocked with mucus or missing entirely. Sperm is still made in the testicles even though it can't pass into the semen made by the prostate gland. Certain fertility treatments and surgical procedures sometimes make it possible for men with CF to become biological parents.
- Lower fertility in women. Although women with CF may be less fertile than other women, it's possible for them to conceive and to have successful pregnancies. Still, pregnancy can worsen the symptoms of CF. Talk with your healthcare professional about the risks.
Other complications
- Thinning of the bones. Cystic fibrosis raises the risk of developing a dangerous thinning of bones called osteoporosis. Joint pain, arthritis and muscle pain also may occur.
- Out of balance electrolytes and dehydration. CF causes saltier sweat, so the balance of minerals in the blood may be upset. This raises the risk for dehydration, especially with exercise or in hot weather. Symptoms of dehydration include a fast heartbeat, extreme tiredness, weakness and low blood pressure.
- Gastroesophageal reflux disease (GERD). Stomach acid repeatedly flows back up into the tube connecting the mouth and stomach, called the esophagus. This backwash is known as acid reflux, and it can irritate the lining of the esophagus.
- Mental health conditions. Having an ongoing medical condition that has no cure may cause fear, depression and anxiety.
- Higher risk of digestive tract cancer. The risk of cancer of the esophagus, stomach, small and large bowel, liver, and pancreas is higher in people with cystic fibrosis. Regular colorectal cancer screening should begin at age 40.
Prevention
If you or your partner have close relatives with cystic fibrosis, you both may choose to have genetic testing before having children. Testing done in a lab on a sample of blood can help find out your risk of having a child with CF.
If you're already pregnant and the genetic test shows that your baby may be at risk of CF, your healthcare professional can do other tests on your unborn child.
Genetic testing isn't for everyone. Before you decide to be tested, talk with a genetic counselor about the mental health impact the test results might have.
Dec. 07, 2024