Overview
A concussion is a mild traumatic brain injury that affects brain function. Effects are often short term and can include headaches and trouble with concentration, memory, balance, mood and sleep.
Concussions usually are caused by an impact to the head or body that is associated with a change in brain function. Not everyone who experiences a blow to the body or head has a concussion.
Some concussions cause the person to lose consciousness, but most do not.
Falls are the most common cause of concussions. Concussions also are common among athletes who play a contact sport, such as American football or soccer. Most people recover fully after a concussion.
Symptoms
The symptoms of a concussion can be subtle and may not occur right away. Symptoms can last for days, weeks or even longer.
Common symptoms after a mild traumatic brain injury are headache, confusion and loss of memory, known as amnesia. The amnesia usually involves forgetting the event that caused the concussion.
Physical symptoms of a concussion may include:
- Headache.
- Ringing in the ears.
- Nausea.
- Vomiting.
- Fatigue or drowsiness.
- Blurry vision.
Other symptoms of a concussion include:
- Confusion or feeling as if in a fog.
- Amnesia surrounding the event.
- Dizziness or "seeing stars."
A witness may observe these symptoms in the person with a concussion:
- Temporary loss of consciousness, though this doesn't always occur.
- Slurred speech.
- Delayed response to questions.
- Dazed appearance.
- Forgetfulness, such as asking the same question over and over.
Some symptoms of a concussion occur right away. But sometimes symptoms may not occur for days after the injury, such as:
- Trouble with concentration and memory.
- Irritability and other personality changes.
- Sensitivity to light and noise.
- Trouble with sleep.
- Feeling emotional or depressed.
- Changes in taste and smell.
Symptoms in children
Concussions can be hard to recognize in infants and toddlers because they can't describe how they feel. Concussion clues may include:
- Dazed appearance.
- Listlessness and tiring easily.
- Irritability and crankiness.
- Loss of balance and unsteady walking.
- Excessive crying.
- Change in eating or sleeping patterns.
- Lack of interest in favorite toys.
- Vomiting.
When to see a doctor
See a healthcare professional within 1 to 2 days if:
- You or your child experiences a head injury, even if emergency care isn't required.
Children and adolescents need to see a healthcare professional trained in evaluating and managing pediatric concussions.
Seek emergency care for an adult or child who experiences a head injury and any of these symptoms:
- Repeated vomiting or nausea.
- A loss of consciousness lasting longer than 30 seconds.
- A headache that gets worse over time.
- Fluid or blood draining from the nose or ears.
- Vision or eye changes. For example, the black parts of the eye, known as the pupils, may be bigger than usual or unequal sizes.
- Ringing in the ears that doesn't go away.
- Weakness in the arms or legs.
- Changes in behavior.
- Confusion or disorientation. For example, the person may not recognize people or places.
- Slurred speech or other changes in speech.
- Obvious changes to mental function.
- Changes in physical coordination, such as stumbling or clumsiness.
- Seizures or convulsions.
- Dizziness that doesn't go away or that goes away and comes back.
- Symptoms that worsen over time.
- Large head bumps or bruises, such as bruises around the eyes or behind the ears. It's especially important to seek emergency care if these symptoms appear in infants under 12 months of age.
When symptoms occur in athletes
Never return to play or vigorous activity immediately following a concussion. Experts recommend that adult, child and adolescent athletes with concussions not return to play on the same day as the injury. Even if a concussion is suspected, experts recommend not returning to activities that can put the athlete at risk of another concussion. Gradual return to learning and physical activity is individual and depends on the symptoms. It should always be supervised by a healthcare professional.
Causes
Types of concussion injuries
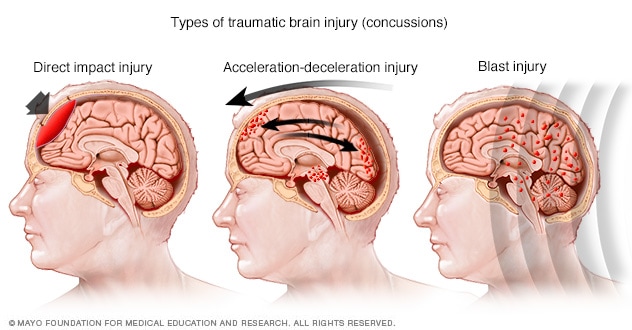
Types of concussion injuries
Common injuries that cause concussions include falls or other direct hits to the head, car accidents, and blast injuries from explosions. These injuries can affect the brain in different ways and cause different types of concussions.
During a concussion, the brain slides back and forth against the inner walls of the skull. This forceful movement can be caused by a violent blow to the head and neck or upper body. It also may be caused by the sudden acceleration or deceleration of the head. This may happen during a car crash, a fall from a bike or from a collision with another player in sports.
These movements injure the brain and affect brain function, usually for a brief period of time. Sometimes a mild traumatic brain injury can lead to bleeding in or around the brain, causing prolonged drowsiness, confusion and, sometimes, death. Anyone who experiences a brain injury needs to be monitored in the hours afterward and seek emergency care if symptoms worsen.
Risk factors
Events and factors that may increase the risk of a concussion include:
- Activities that can lead to falls, especially in young children and older adults.
- High-risk sports such as American football, hockey, soccer, rugby, boxing or other contact sports.
- Not using proper safety equipment and supervision when playing high-risk sports.
- Auto accidents.
- Pedestrian or bicycle accidents.
- Military combat.
- Physical abuse.
Having had a previous concussion also increases the risk of having another.
Complications
Potential complications of concussion include:
- Post-traumatic headaches. Some people experience concussion-related headaches for several days to weeks after a brain injury.
- Post-traumatic vertigo. Some people experience a sense of spinning or dizziness for days or weeks after a brain injury.
- Persistent post-concussive symptoms, also known as post-concussion syndrome. A small number of people may have multiple symptoms that last longer than expected. Longer lasting symptoms may include headaches, dizziness and trouble with thinking. If these symptoms persist beyond three months, they're called persistent post-concussive symptoms.
- Effects of multiple brain injuries. Researchers are studying the effects of repeated head injuries that don't cause symptoms, known as subconcussive injury. At this time, there's no conclusive evidence that these repeated brain injuries affect brain function.
- Second impact syndrome. Rarely, experiencing a second concussion before symptoms of a first concussion go away may result in rapid brain swelling. This can lead to death. It's important that athletes never return to sports while they're still experiencing symptoms of concussion.
Prevention
These tips may help you prevent or minimize the risk of a concussion:
-
Wear protective gear during sports and other recreational activities. Make sure the equipment fits properly, is well maintained and is worn correctly. Follow the rules of the game and practice good sportsmanship.
Be sure to wear a helmet when bicycling, motorcycling, snowboarding or doing any activity that may result in a head injury.
- Buckle your seat belt. Wearing a seat belt may prevent serious injury, including head injury, during a traffic accident.
- Make your home safe. Keep your home well lit. Keep your floors free of anything that might cause you to trip and fall. Falls around the home are a leading cause of head injury.
- Protect your children. To help lessen the risk of head injuries in children, block off stairways and install window guards.
- Exercise regularly. Exercise strengthens your leg muscles and improves your balance.
- Educate others about concussions. Educate coaches, athletes, parents and others about concussions to help spread awareness. Coaches and parents also can help encourage good sportsmanship.
Jan. 12, 2024