Diagnosis
Kidney disease FAQs
Nephrologist Andrew Bentall, M.D., answers the most frequently asked questions about kidney disease.
Living with diabetes is difficult, thinking about what you eat. But controlling the sugar levels are really important for helping kidney function and specifically slowing down any damage to the kidneys. Newer drugs that have come out in the last couple years can help with this, as well as working with your primary care physician or endocrinologist with your current therapies to get better sugar control.
We really want to help your health and so losing weight can be a key component to reducing your risk of progressing with kidney disease. Reducing calorie intake, which is either smaller portions, less snacking in between meals, and then thinking about burning calories with increasing your exercise, are great steps forward in starting that journey towards weight loss.
We look to get blood pressure less than 130 systolic, that's the top number. And less than 80 diastolic, that's the bottom number, on blood pressure readings. There are a number of different drugs that we can use to do this. And this will help both with your cardiovascular health, but slowing down any kidney disease progression over time as well.
There are two different types of dialysis: hemodialysis, which is done through cleaning the blood through a machine, which you attend a dialysis center three times a week for about four hours each time. It can be done at home in certain circumstances. Or peritoneal dialysis, where fluid gets put into your tummy, takes out the toxins and is drained. And that can be done either during the day or overnight on a machine. The benefits and risks of these are individualized, as some people are able to do the treatment at home or need to go to a treatment center for this. It also depends on your location and how close the nearest dialysis centers are.
The kidney transplant works in the same way as your own kidneys do, with the blood coming through the transplant, filtering it and the urine coming out. The kidney transplant is protected by the anti-rejection medication, so your body doesn't attack it. And we leave your own kidneys in because they eventually shrivel down and don't function anymore. You don't want more surgery than you need.
For a kidney transplant at the moment, taking anti-rejection drugs is an everyday, lifelong occurrence. These can come with side effects. But current research is looking to try and minimize or come off anti-rejection drugs with specific research protocols at the moment.
We really want to partner with you to get the best outcomes for you, so that chronic kidney disease doesn't affect you as much as it can. Controlling your blood pressure and therefore monitoring that at home, taking your medications regularly, and letting us know about side effects is a really important part in partnering and helping you to have a good quality of life living with chronic kidney disease.
Kidney biopsy
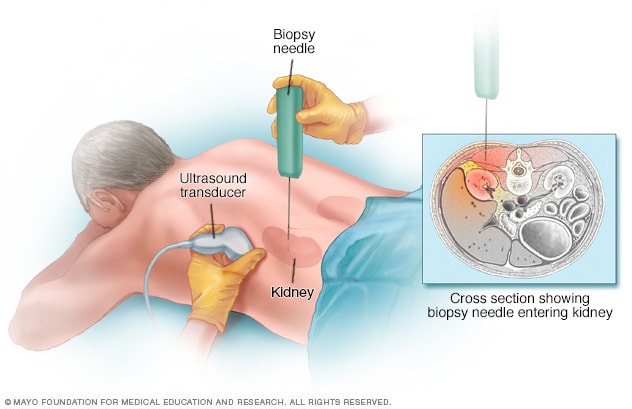
Kidney biopsy
During a kidney biopsy, a healthcare professional uses a needle to remove a small sample of kidney tissue for lab testing. The biopsy needle is put through the skin to the kidney. The procedure often uses an imaging device, such as an ultrasound transducer, to guide the needle.
As a first step toward diagnosis of kidney disease, your doctor discusses your personal and family history with you. Among other things, your doctor might ask questions about whether you've been diagnosed with high blood pressure, if you've taken a medication that might affect kidney function, if you've noticed changes in your urinary habits and whether you have family members who have kidney disease.
Next, your doctor performs a physical exam, checking for signs of problems with your heart or blood vessels, and conducts a neurological exam.
For kidney disease diagnosis, you might also need certain tests and procedures to determine how severe your kidney disease is (stage). Tests might include:
- Blood tests. Kidney function tests look for the level of waste products, such as creatinine and urea, in your blood.
- Urine tests. Analyzing a sample of your urine can reveal abnormalities that point to chronic kidney failure and help identify the cause of chronic kidney disease.
- Imaging tests. Your doctor might use ultrasound to assess your kidneys' structure and size. Other imaging tests might be used in some cases.
- Removing a sample of kidney tissue for testing. Your doctor might recommend a kidney biopsy, which involves removing a sample of kidney tissue. Kidney biopsy is often done with local anesthesia using a long, thin needle that's inserted through your skin and into your kidney. The biopsy sample is sent to a lab for testing to help determine what's causing your kidney problem.
More Information
Treatment
Start Your Donor Evaluation
Get started as a living kidney or liver donor by completing this health history questionnaire.
Kidney transplant
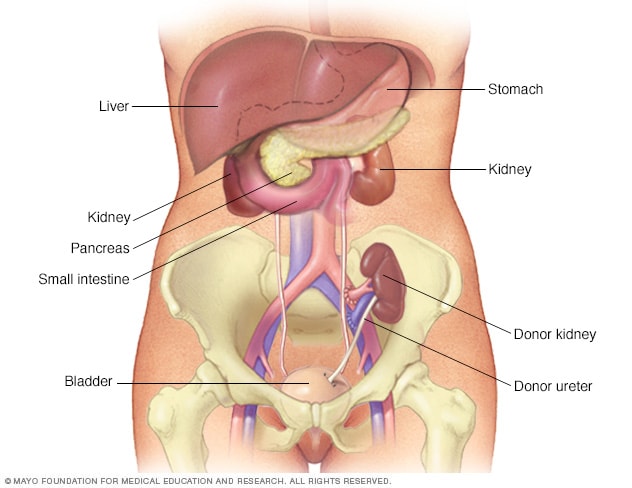
Kidney transplant
During kidney transplant surgery, the donor kidney is placed in your lower abdomen. Blood vessels of the new kidney are attached to blood vessels in the lower part of your abdomen, just above one of your legs. The new kidney's urine tube (ureter) is connected to your bladder. Unless they are causing complications, your own kidneys are left in place.
Depending on the cause, some types of kidney disease can be treated. Often, though, chronic kidney disease has no cure.
Treatment usually consists of measures to help control signs and symptoms, reduce complications, and slow progression of the disease. If your kidneys become severely damaged, you might need treatment for end-stage kidney disease.
Treating the cause
Your doctor will work to slow or control the cause of your kidney disease. Treatment options vary depending on the cause. But kidney damage can continue to worsen even when an underlying condition, such as diabetes mellitus or high blood pressure, has been controlled.
Treating complications
Kidney disease complications can be controlled to make you more comfortable. Treatments might include:
-
High blood pressure medications. People with kidney disease can have worsening high blood pressure. Your doctor might recommend medications to lower your blood pressure — commonly angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers — and to preserve kidney function.
High blood pressure medications can initially decrease kidney function and change electrolyte levels, so you might need frequent blood tests to monitor your condition. Your doctor may also recommend a water pill (diuretic) and a low-salt diet.
- Medications to relieve swelling. People with chronic kidney disease often retain fluids. This can lead to swelling in the legs as well as high blood pressure. Medications called diuretics can help maintain the balance of fluids in your body.
- Medications to treat anemia. Supplements of the hormone erythropoietin (uh-rith-roe-POI-uh-tin), sometimes with added iron, help produce more red blood cells. This might relieve fatigue and weakness associated with anemia.
- Medications to lower cholesterol levels. Your doctor might recommend medications called statins to lower your cholesterol. People with chronic kidney disease often have high levels of bad cholesterol, which can increase the risk of heart disease.
- Medications to protect your bones. Calcium and vitamin D supplements can help prevent weak bones and lower your risk of fracture. You might also take medication known as a phosphate binder to lower the amount of phosphate in your blood and protect your blood vessels from damage by calcium deposits (calcification).
- A lower protein diet to minimize waste products in your blood. As your body processes protein from foods, it creates waste products that your kidneys must filter from your blood. To reduce the amount of work your kidneys must do, your doctor might recommend eating less protein. A registered dietitian can suggest ways to lower your protein intake while still eating a healthy diet.
Your doctor might recommend regular follow-up testing to see whether your kidney disease remains stable or progresses.
Treatment for end-stage kidney disease
If your kidneys can't keep up with waste and fluid clearance on their own and you develop complete or near-complete kidney failure, you have end-stage kidney disease. At that point, you need dialysis or a kidney transplant.
-
Dialysis. Dialysis artificially removes waste products and extra fluid from your blood when your kidneys can no longer do this. In hemodialysis, a machine filters waste and excess fluids from your blood.
In peritoneal dialysis, a thin tube inserted into your abdomen fills your abdominal cavity with a dialysis solution that absorbs waste and excess fluids. After a time, the dialysis solution drains from your body, carrying the waste with it.
-
Kidney transplant. A kidney transplant involves surgically placing a healthy kidney from a donor into your body. Transplanted kidneys can come from deceased or living donors.
After a transplant, you'll need to take medications for the rest of your life to keep your body from rejecting the new organ. You don't need to be on dialysis to have a kidney transplant.
For some who choose not to have dialysis or a kidney transplant, a third option is to treat your kidney failure with conservative measures. Conservative measures likely will include symptom management, advance care planning and care to keep you comfortable (palliative care).
Kidney Disease: How kidneys work, Hemodialysis, and Peritoneal dialysis
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
As part of your treatment for chronic kidney disease, your doctor might recommend a special diet to help support your kidneys and limit the work they must do. Ask your doctor for a referral to a registered dietitian who can analyze your diet and suggest ways to make your diet easier on your kidneys.
Depending on your situation, kidney function and overall health, dietary recommendations might include the following:
- Avoid products with added salt. Lower the amount of sodium you eat each day by avoiding products with added salt, including many convenience foods, such as frozen dinners, canned soups and fast foods. Other foods with added salt include salty snack foods, canned vegetables, and processed meats and cheeses.
- Choose lower potassium foods. High-potassium foods include bananas, oranges, potatoes, spinach and tomatoes. Examples of low-potassium foods include apples, cabbage, carrots, green beans, grapes and strawberries. Be aware that many salt substitutes contain potassium, so you generally should avoid them if you have kidney failure.
- Limit the amount of protein you eat. Your registered dietitian will estimate how many grams of protein you need each day and make recommendations based on that amount. High-protein foods include lean meats, eggs, milk, cheese and beans. Low-protein foods include vegetables, fruits, breads and cereals.
More Information
Coping and support
Receiving a diagnosis of chronic kidney disease can be worrisome. To help you cope with your feelings, consider:
- Connecting with other people who have kidney disease. They can understand what you're feeling and offer unique support. Ask your doctor about support groups in your area. Or contact organizations such as the American Association of Kidney Patients, the National Kidney Foundation or the American Kidney Fund for groups in your area.
- Maintaining your normal routine, when possible. Try to keep doing the activities you enjoy and continue working, if your condition allows. This can help you cope with feelings of sadness or loss that you might have.
- Being active most days of the week. With your doctor's advice, aim for at least 30 minutes of physical activity most days of the week. This can help you cope with fatigue and stress.
- Talking with someone you trust. You might have a friend or family member who is a good listener. Or you may find it helpful to talk with a faith leader or someone else you trust. Ask your doctor for a referral to a social worker or counselor.
Preparing for your appointment
You'll likely start by seeing your primary care doctor. If lab tests reveal that you have kidney damage, you might be referred to a doctor who specializes in kidney problems (nephrologist).
What you can do
To get ready for your appointment, ask if there's anything you need to do ahead of time, such as limit your diet. Then make a list of:
- Your symptoms, including any that seem unrelated to your kidneys or urinary function, and when they began
- All your medications, vitamins or other supplements you take, including doses
- Other medical conditions you have and relatives with kidney disease
- Questions to ask about your condition
Take a family member or friend along, if possible, to help you remember the information you receive. Or use a recorder during your visit.
For chronic kidney disease, some basic questions to ask include:
- What's the level of damage to my kidneys?
- Is my kidney function worsening?
- Do I need more tests?
- What's causing my condition?
- Can the damage to my kidneys be reversed?
- What are my treatment options?
- What are the potential side effects of each treatment?
- I have these other health conditions. How can I best manage them together?
- Do I need to eat a special diet?
- Can you refer me to a dietitian who can help me plan my meals?
- Are there brochures or other printed material I can have? What websites do you recommend?
- How often do I need to have my kidney function tested?
Don't hesitate to ask other questions as they occur to you.
What to expect from your doctor
Your doctor is likely to ask you questions, such as:
- How long have you had symptoms?
- Have you been diagnosed or treated for high blood pressure?
- Have you noticed changes in your urinary habits?
Sept. 06, 2023