Diagnosis
Receiving a mammogram
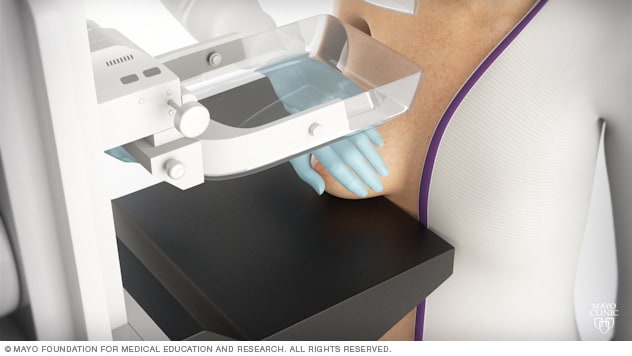
Receiving a mammogram
During a mammogram, you stand in front of an X-ray machine designed for mammography. A technician places your breast on a platform and positions the platform to match your height. The technician helps you position your head, arms and torso to allow an unobstructed view of your breast.
Breast MRI
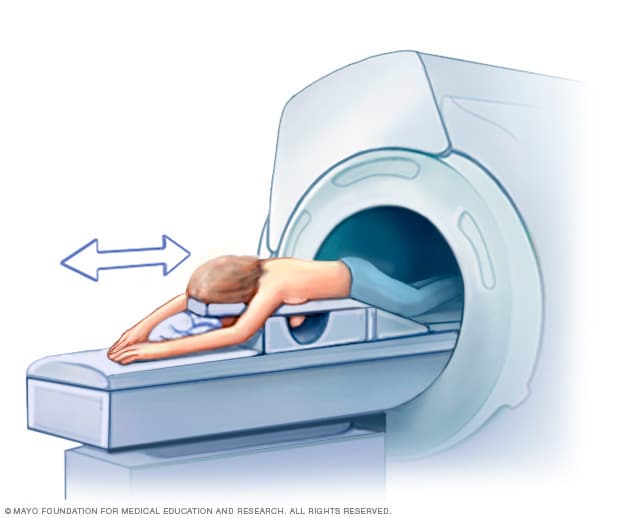
Breast MRI
Getting a breast MRI involves lying face down on a padded scanning table. The breasts fit into a hollow space in the table. The hollow has coils that get signals from the MRI. The table slides into the large opening of the MRI machine.
Core needle biopsy
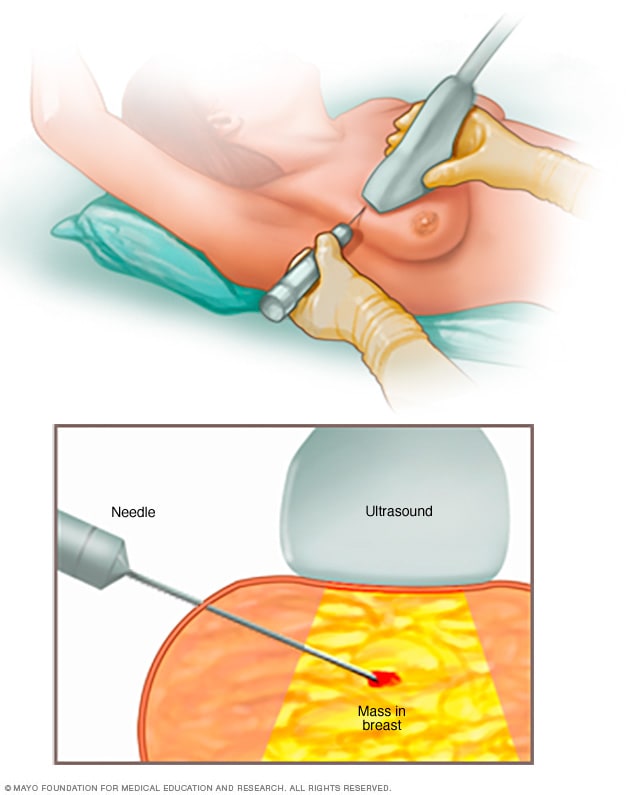
Core needle biopsy
A core needle biopsy uses a long, hollow tube to obtain a sample of tissue. Here, a biopsy of a suspicious breast lump is being done. The sample is sent to a lab for testing by doctors called pathologists. They specialize in examining blood and body tissue.
Breast cancer diagnosis often begins with an exam and a discussion of your symptoms. Imaging tests can look at the breast tissue for anything that's not typical. To confirm whether there is cancer or not, a sample of tissue is removed from the breast for testing.
Breast exam
During a clinical breast exam, a healthcare professional looks at the breasts for anything that's not typical. This might include changes in the skin or to the nipple. Then the health professional feels the breasts for lumps. The health professional also feels along the collarbones and around the armpits for lumps.
Mammogram
A mammogram is an X-ray of the breast tissue. Mammograms are commonly used to screen for breast cancer. If a screening mammogram finds something concerning, you might have another mammogram to look at the area more closely. This more-detailed mammogram is called a diagnostic mammogram. It's often used to look closely at both breasts.
Breast ultrasound
Ultrasound uses sound waves to make pictures of structures inside the body. A breast ultrasound may give your healthcare team more information about a breast lump. For example, an ultrasound might show whether the lump is a solid mass or a fluid-filled cyst. The healthcare team uses this information to decide what tests you might need next.
Breast MRI
MRI machines use a magnetic field and radio waves to create pictures of the inside of the body. A breast MRI can make more-detailed pictures of the breast. Sometimes this method is used to look closely for any other areas of cancer in the affected breast. It also might be used to look for cancer in the other breast. Before a breast MRI, you usually receive an injection of dye. The dye helps the tissue show up better in the images.
Removing a sample of breast cells for testing
A biopsy is a procedure to remove a sample of tissue for testing in a lab. To get the sample, a healthcare professional puts a needle through the skin and into the breast tissue. The health professional guides the needle using images created with X-rays, ultrasound or another type of imaging. Once the needle reaches the right place, the health professional uses the needle to draw out tissue from the breast. Often, a marker is placed in the spot where the tissue sample was removed. The small metal marker will show up on imaging tests. The marker helps your healthcare team monitor the area of concern.
Testing cells in the lab
The tissue sample from a biopsy goes to a lab for testing. Tests can show whether the cells in the sample are cancerous. Other tests give information about the type of cancer and how quickly it's growing. Special tests give more details about the cancer cells. For example, tests might look for hormone receptors on the surface of the cells. Your healthcare team uses the results from these tests to make a treatment plan.
Staging breast cancer
Once your healthcare team diagnoses your breast cancer, you may have other tests to figure out the extent of the cancer. This is called the cancer's stage. Your healthcare team uses your cancer's stage to understand your prognosis.
Complete information about your cancer's stage may not be available until after you undergo breast cancer surgery.
Tests and procedures used to stage breast cancer may include:
- Blood tests, such as a complete blood count and tests to show how well the kidneys and liver are working.
- Bone scan.
- CT scan.
- MRI.
- Positron emission tomography scan, also called a PET scan.
Not everyone needs all of these tests. Your healthcare team picks the right tests based on your specific situation.
Breast cancer stages range from 0 to 4. A lower number means the cancer is less advanced and more likely to be cured. Stage 0 breast cancer is cancer that is contained within a breast duct. It hasn't broken out to invade the breast tissue yet. As the cancer grows into the breast tissue and gets more advanced, the stages get higher. A stage 4 breast cancer means that the cancer has spread to other parts of the body.
More Information
Treatment
Breast cancer treatment often starts with surgery to remove the cancer. Most people with breast cancer will have other treatments after surgery, such as radiation, chemotherapy and hormone therapy. Some people may have chemotherapy or hormone therapy before surgery. These medicines can help shrink the cancer and make it easier to remove.
Your treatment plan will depend on your particular breast cancer. Your healthcare team considers the stage of the cancer, how quickly it's growing and whether the cancer cells are sensitive to hormones. Your care team also considers your overall health and what you prefer.
There are many options for breast cancer treatment. It can feel overwhelming to consider all the options and make complex decisions about your care. Consider seeking a second opinion from a breast specialist in a breast center or clinic. Talk to breast cancer survivors who have faced the same decision.
Breast cancer surgery
Lumpectomy
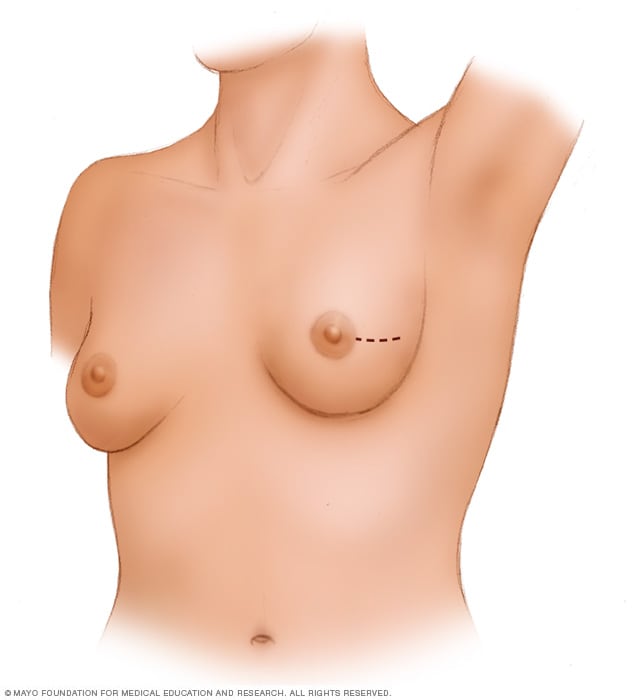
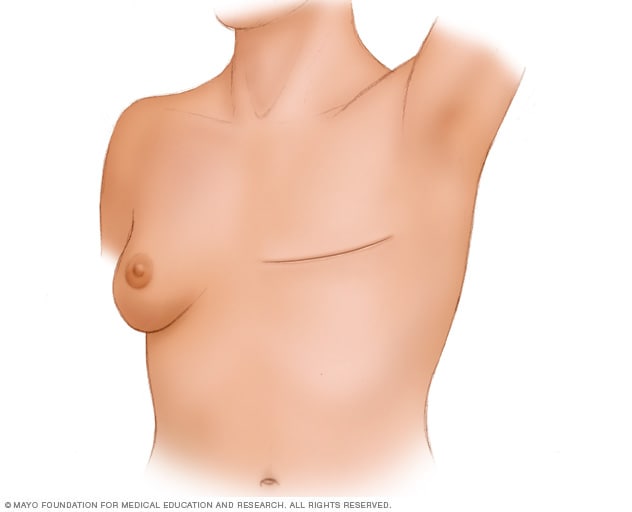
Lumpectomy
A lumpectomy involves removing the cancer and some of the healthy tissue that surrounds it. This illustration shows one possible incision that can be used for this procedure, though your surgeon will determine the approach that's best for your particular situation.
Mastectomy
Mastectomy
During a total mastectomy, the surgeon removes the breast tissue, nipple, areola and skin. This procedure also is known as a simple mastectomy. Other mastectomy procedures may leave some parts of the breast, such as the skin or the nipple. Surgery to create a new breast is optional. It may be done at the same time as mastectomy surgery or it can be done later.
Sentinel node biopsy
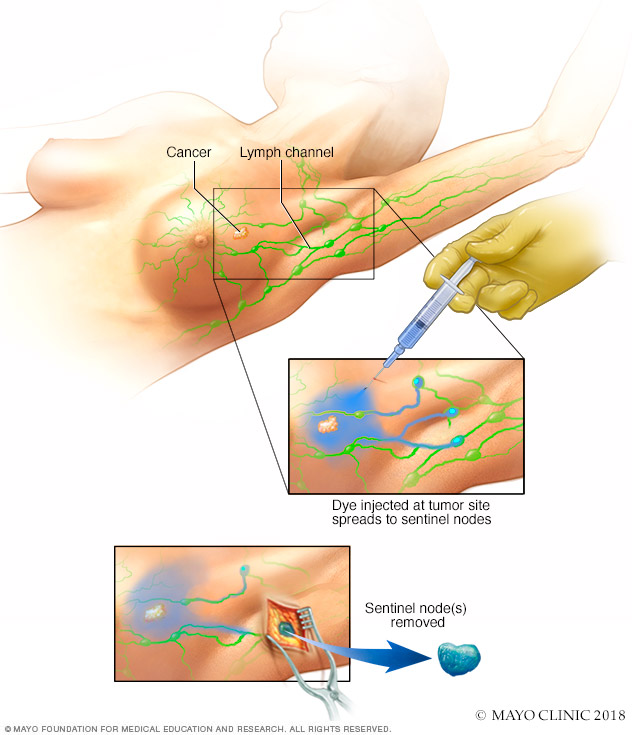
Sentinel node biopsy
Sentinel node biopsy identifies the first few lymph nodes into which a tumor drains. The surgeon uses a harmless dye and a weak radioactive solution to locate the sentinel nodes. The nodes are removed and tested for signs of cancer.
Breast cancer surgery typically involves a procedure to remove the breast cancer and a procedure to remove some nearby lymph nodes. Operations used to treat breast cancer include:
-
Removing the breast cancer. A lumpectomy is surgery to remove the breast cancer and some of the healthy tissue around it. The rest of the breast tissue isn't removed. Other names for this surgery are breast-conserving surgery and wide local excision. Most people who have a lumpectomy also have radiation therapy.
Lumpectomy might be used to remove a small cancer. Sometimes you can have chemotherapy before surgery to shrink the cancer so that lumpectomy is possible.
-
Removing all of the breast tissue. A mastectomy is surgery to remove all breast tissue from a breast. The most common mastectomy procedure is total mastectomy, also called simple mastectomy. This procedure removes all of the breast, including the lobules, ducts, fatty tissue and some skin, including the nipple and areola.
Mastectomy might be used to remove a large cancer. It also might be needed when there are multiple areas of cancer within one breast. You might have a mastectomy if you can't have or don't want radiation therapy after surgery.
Some newer types of mastectomy procedures might not remove the skin or nipple. For instance, a skin-sparing mastectomy leaves some skin. A nipple-sparing mastectomy leaves the nipple and the skin around it, called the areola. These newer operations can improve the look of the breast after surgery, but they aren't options for everyone.
- Removing a few lymph nodes. A sentinel node biopsy is an operation to take out some lymph nodes for testing. When breast cancer spreads, it often goes to the nearby lymph nodes first. To see if the cancer has spread, a surgeon removes some of the lymph nodes near the cancer. If no cancer is found in those lymph nodes, the chance of finding cancer in any of the other lymph nodes is small. No other lymph nodes need to be removed.
- Removing several lymph nodes. Axillary lymph node dissection is an operation to remove many lymph nodes from the armpit. Your breast cancer surgery might include this operation if imaging tests show the cancer has spread to the lymph nodes. It also might be used if cancer is found in a sentinel node biopsy.
- Removing both breasts. Some people who have cancer in one breast may choose to have their other breast removed, even if it doesn't have cancer. This procedure is called a contralateral prophylactic mastectomy. It might be an option if you have a high risk of getting cancer in the other breast. The risk might be high if you have a strong family history of cancer or have DNA changes that increase the risk of cancer. Most people with breast cancer in one breast will never get cancer in the other breast.
Complications of breast cancer surgery depend on the procedures you choose. All operations have a risk of pain, bleeding and infection. Removing lymph nodes in the armpit carries a risk of arm swelling, called lymphedema.
You may choose to have breast reconstruction after mastectomy surgery. Breast reconstruction is surgery to restore shape to the breast. Options might include reconstruction with a breast implant or reconstruction using your own tissue. Consider asking your healthcare team for a referral to a plastic surgeon before your breast cancer surgery.
Radiation therapy
Radiation therapy
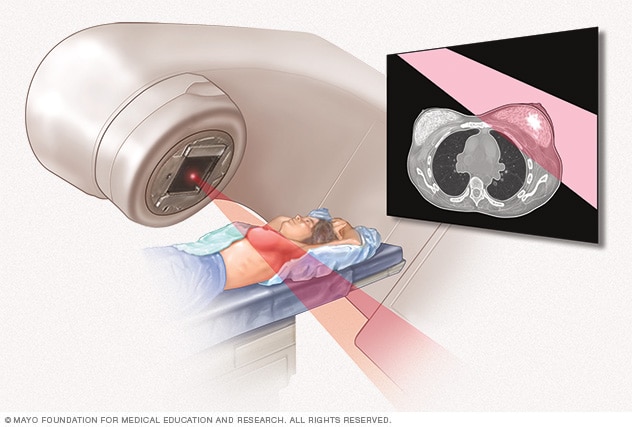
Radiation therapy
External beam radiation uses high-powered beams of energy to kill cancer cells. Beams of radiation are precisely aimed at the cancer using a machine that moves around your body.
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources.
For breast cancer treatment, the radiation is often external beam radiation. During this type of radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body. Less often, the radiation can be placed inside the body. This type of radiation is called brachytherapy.
Radiation therapy is often used after surgery. It can kill any cancer cells that might be left after surgery. The radiation lowers the risk of the cancer coming back.
Side effects of radiation therapy include feeling very tired and having a sunburn-like rash where the radiation is aimed. Breast tissue also may look swollen or feel more firm. Rarely, more-serious problems can happen. These include damage to the heart or lungs. Very rarely, a new cancer can grow in the treated area.
Chemotherapy
Chemotherapy treats cancer with strong medicines. Many chemotherapy medicines exist. Treatment often involves a combination of chemotherapy medicines. Most are given through a vein. Some are available in pill form.
Chemotherapy for breast cancer is often used after surgery. It can kill any cancer cells that might remain and lower the risk of the cancer coming back.
Sometimes chemotherapy is given before surgery. The chemotherapy might shrink the breast cancer so that it's easier to remove. Chemotherapy before surgery also might control cancer that spreads to the lymph nodes. If the lymph nodes no longer show signs of cancer after chemotherapy, surgery to remove many lymph nodes might not be needed. How the cancer responds to chemotherapy before surgery helps the healthcare team make decisions about what treatments might be needed after surgery.
When the cancer spreads to other parts of the body, chemotherapy can help control it. Chemotherapy may relieve symptoms of an advanced cancer, such as pain.
Chemotherapy side effects depend on which medicines you receive. Common side effects include hair loss, nausea, vomiting, feeling very tired and having an increased risk of getting an infection. Rare side effects can include premature menopause and nerve damage. Very rarely, certain chemotherapy medicines can cause blood cell cancer.
Hormone therapy
Hormone therapy uses medicines to block certain hormones in the body. It's a treatment for breast cancers that are sensitive to the hormones estrogen and progesterone. Healthcare professionals call these cancers estrogen receptor positive and progesterone receptor positive. Cancers that are sensitive to hormones use the hormones as fuel for their growth. Blocking the hormones can cause the cancer cells to shrink or die.
Hormone therapy is often used after surgery and other treatments. It can lower the risk that the cancer will come back.
If the cancer spreads to other parts of the body, hormone therapy can help control it.
Treatments that can be used in hormone therapy include:
- Medicines that block hormones from attaching to cancer cells. These medicines are called selective estrogen receptor modulators.
- Medicines that stop the body from making estrogen after menopause. These medicines are called aromatase inhibitors.
- Surgery or medicines to stop the ovaries from making hormones.
Hormone therapy side effects depend on the treatment you receive. The side effects can include hot flashes, night sweats and vaginal dryness. More-serious side effects include a risk of bone thinning and blood clots.
Targeted therapy
Targeted therapy uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die.
The most common targeted therapy medicines for breast cancer target the protein HER2. Some breast cancer cells make extra HER2. This protein helps the cancer cells grow and survive. Targeted therapy medicine attacks the cells that are making extra HER2 and doesn't hurt healthy cells.
Many other targeted therapy medicines exist for treating breast cancer. Your cancer cells may be tested to see whether these medicines might help you.
Targeted therapy medicines can be used before surgery to shrink a breast cancer and make it easier to remove. Some are used after surgery to lower the risk that the cancer will come back. Others are used only when the cancer has spread to other parts of the body.
Immunotherapy
Immunotherapy is a treatment with medicine that helps the body's immune system to kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn't be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells.
Immunotherapy might be an option for treating triple-negative breast cancer. Triple-negative breast cancer means that the cancer cells don't have receptors for estrogen, progesterone or HER2.
Palliative care
Palliative care is a special type of healthcare that helps you feel better when you have a serious illness. If you have cancer, palliative care can help relieve pain and other symptoms. A team of healthcare professionals provides palliative care. The team can include doctors, nurses and other specially trained professionals. Their goal is to improve quality of life for you and your family.
Palliative care specialists work with you, your family and your care team to help you feel better. They provide an extra layer of support while you have cancer treatment. You can have palliative care at the same time as strong cancer treatments, such as surgery, chemotherapy or radiation therapy.
When palliative care is used along with all of the other appropriate treatments, people with cancer may feel better and live longer.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Alternative medicine
No alternative medicine treatments have been found to cure breast cancer. But complementary and alternative medicine therapies may help you cope with side effects of treatment.
Alternative medicine for fatigue
Many people with breast cancer have fatigue during and after treatment. This feeling of being very tired and worn down can continue for years. When combined with care from your healthcare team, complementary and alternative medicine therapies may help relieve fatigue.
Talk with your healthcare team about:
- Expressing your feelings. Find an activity that allows you to write about or discuss your emotions. Examples include writing in a journal, participating in a support group or talking to a counselor.
- Gentle exercise. If you get the OK from your healthcare team, start with gentle exercise a few times a week. Add more exercise, as you feel up to it. Consider walking, swimming, yoga and tai chi.
- Managing stress. Take control of the stress in your daily life. Try stress-reduction techniques such as muscle relaxation, visualization, and spending time with friends and family.
Coping and support
Some breast cancer survivors say their diagnosis felt overwhelming at first. It can be stressful to feel overwhelmed at the same time you need to make important decisions about your treatment. In time, you'll find ways to cope with your feelings. Until you find what works for you, it might help to:
Learn enough about your breast cancer to make decisions about your care
If you'd like to know more about your breast cancer, ask your healthcare team for the details of your cancer. Write down the type, stage and hormone receptor status. Ask for good sources of information where you can learn more about your treatment options.
Knowing more about your cancer and your options may help you feel more confident when making treatment decisions. Still, some people don't want to know the details of their cancer. If this is how you feel, let your care team know that too.
Talk with other breast cancer survivors
You may find it helpful and encouraging to talk to others who have been diagnosed with breast cancer. Contact a cancer support organization in your area to find out about support groups near you or online. In the United States, you might start with the American Cancer Society.
Find someone to talk with about your feelings
Find a friend or family member who is a good listener. Or talk with a clergy member or counselor. Ask your healthcare team for a referral to a counselor or other professional who works with people who have cancer.
Keep your friends and family close
Your friends and family can provide a crucial support network for you during your cancer treatment.
As you begin telling people about your breast cancer diagnosis, you'll likely get many offers for help. Think ahead about things you may want help with. Examples include listening when you want to talk or helping you with preparing meals.
Preparing for your appointment
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you. If an exam or imaging test shows you might have breast cancer, your healthcare team will likely refer you to a specialist.
Specialists who care for people with breast cancer include:
- Breast health specialists.
- Breast surgeons.
- Doctors who specialize in diagnostic tests, such as mammograms, called radiologists.
- Doctors who specialize in treating cancer, called oncologists.
- Doctors who treat cancer with radiation, called radiation oncologists.
- Genetic counselors.
- Plastic surgeons.
What you can do to prepare
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Write down your family history of cancer. Note any family members who have had cancer. Note how each member is related to you, the type of cancer, the age at diagnosis and whether each person survived.
- Make a list of all medicines, vitamins or supplements that you're taking.
- Keep all of your records that relate to your cancer diagnosis and treatment. Organize your records in a binder or folder that you can take to your appointments.
- Consider taking a family member or friend along. Sometimes it can be difficult to absorb all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your healthcare professional.
Questions to ask your doctor
Your time with your healthcare professional is limited. Prepare a list of questions so that you can make the most of your time together. List your questions from most important to least important in case time runs out. For breast cancer, some basic questions to ask include:
- What type of breast cancer do I have?
- What is the stage of my cancer?
- Can you explain my pathology report to me? Can I have a copy for my records?
- Do I need any more tests?
- What treatment options are available for me?
- What are the benefits from each treatment you recommend?
- What are the side effects of each treatment option?
- Will treatment cause menopause?
- How will each treatment affect my daily life? Can I continue working?
- Is there one treatment you recommend over the others?
- How do you know that these treatments will benefit me?
- What would you recommend to a friend or family member in my situation?
- How quickly do I need to make a decision about cancer treatment?
- What happens if I don't want cancer treatment?
- What will cancer treatment cost?
- Does my insurance plan cover the tests and treatment you're recommending?
- Should I seek a second opinion? Will my insurance cover it?
- Are there any brochures or other printed material that I can take with me? What websites or books do you recommend?
- Are there any clinical trials or newer treatments that I should consider?
In addition to the questions that you've prepared, don't hesitate to ask other questions you think of during your appointment.
What to expect from your doctor
Be prepared to answer some questions about your symptoms and your health, such as:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
Jan. 10, 2025
- Cancer facts and figures 2023. American Cancer Society. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html. Accessed Aug. 9, 2023.
- Abraham J, et al., eds. Breast cancer. In: The Bethesda Handbook of Clinical Oncology. 6th ed. Kindle edition. Wolters Kluwer; 2023. Accessed March 30, 2023.
- Breast cancer. Cancer.Net. https://www.cancer.net/cancer-types/breast-cancer/view-all. Accessed Aug. 2, 2023.
- Mukwende M, et al. Erythema. In: Mind the Gap: A Handbook of Clinical Signs in Black and Brown Skin. St. George's University of London; 2020. https://www.blackandbrownskin.co.uk/mindthegap. Accessed Aug. 10, 2023.
- Townsend CM Jr, et al. Diseases of the breast. In: Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 21st ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed Aug. 2, 2023.
- Breast cancer risk reduction. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1420. Accessed Aug. 2, 2023.
- Breast cancer prevention (PDQ) – Patient version. National Cancer Institute. https://www.cancer.gov/types/breast/patient/breast-prevention-pdq. Accessed Aug. 2, 2023.
- Breast cancer. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1419. Accessed Aug. 2, 2023.
- Klimberg VS, et al., eds. Breast cancer diagnosis and techniques for biopsy. In: Bland and Copeland's The Breast: Comprehensive Management of Benign and Malignant Diseases. 6th ed. Elsevier; 2024. https://www.clinicalkey.com. Accessed Aug. 2, 2023.
- Palliative care. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1454. Accessed Aug. 2, 2023.
- Cancer-related fatigue. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=3&id=1424. Accessed Aug. 2, 2023.
- Breast SPOREs. National Cancer Institute. https://trp.cancer.gov/spores/breast.htm. Accessed Aug. 9, 2023.
- Ami TR. Allscripts EPSi. Mayo Clinic. Jan. 31, 2023.
- Ami TR. Allscripts EPSi. Mayo Clinic. April 5, 2023.
- Member institutions. Alliance for Clinical Trials in Oncology. https://www.allianceforclinicaltrialsinoncology.org/main/public/standard.xhtml?path=%2FPublic%2FInstitutions. Accessed Aug. 9, 2023.
- Giridhar KV (expert opinion). Mayo Clinic. Oct. 18, 2023.
Related
Associated Procedures
News from Mayo Clinic