Diagnosis
Meningioma

Meningioma
This contrast-enhanced MRI scan of a person's head shows a meningioma. This meningioma has grown large enough to push down into the brain tissue.
Brain tumor MRI

Brain tumor MRI
Brain tumor imaging
If your health care provider thinks you might have a brain tumor, you'll need a number of tests and procedures to be sure. These might include:
- A neurological exam. A neurological exam tests different parts of your brain to see how they're working. This exam may include checking your vision, hearing, balance, coordination, strength and reflexes. If you have trouble in one or more areas, this is a clue for your health care provider. A neurological exam doesn't detect a brain tumor. But it helps your provider understand what part of your brain might be having a problem.
- Head CT scan. A computed tomography scan, also called a CT scan, uses X-rays to make pictures. It's widely available, and results come back quickly. So CT might be the first imaging test that's done if you have headaches or other symptoms that have many possible causes. A CT scan can detect problems in and around your brain. The results give your health care provider clues to decide what test to do next. If your provider thinks your CT scan shows a brain tumor, you might need a brain MRI.
-
Brain MRI. Magnetic resonance imaging, also called MRI, uses strong magnets to create pictures of the inside of the body. MRI is often used to detect brain tumors because it shows the brain more clearly than do other imaging tests.
Often a dye is injected into a vein in the arm before an MRI. The dye makes clearer pictures. This makes it easier to see smaller tumors. It can help your health care team see the difference between a brain tumor and healthy brain tissue.
Sometimes you need a special type of MRI to create more-detailed pictures. One example is functional MRI. This special MRI shows which parts of the brain control speaking, moving and other important tasks. This helps your health care provider plan surgery and other treatments.
Another special MRI test is magnetic resonance spectroscopy. This test uses MRI to measure levels of certain chemicals in the tumor cells. Having too much or too little of the chemicals might tell your health care team about the kind of brain tumor you have.
Magnetic resonance perfusion is another special type of MRI. This test uses MRI to measure the amount of blood in different parts of the brain tumor. The parts of the tumor that have a higher amount of blood may be the most active parts of the tumor. Your health care team uses this information to plan your treatment.
-
PET scan of the brain. A positron emission tomography scan, also called a PET scan, can detect some brain tumors. A PET scan uses a radioactive tracer that's injected into a vein. The tracer travels through the blood and attaches to brain tumor cells. The tracer makes the tumor cells stand out on the pictures taken by the PET machine. Cells that are dividing and multiplying quickly will take up more of the tracer.
A PET scan may be most helpful for detecting brain tumors that are growing quickly. Examples include glioblastomas and some oligodendrogliomas. Brain tumors that grow slowly might not be detected on a PET scan. Brain tumors that aren't cancerous tend to grow more slowly, so PET scans are less useful for benign brain tumors. Not everyone with a brain tumor needs a PET scan. Ask your health care provider whether you need at PET scan.
-
Collecting a sample of tissue. A brain biopsy is a procedure to remove a sample of brain tumor tissue for testing in a lab. Often a surgeon gets the sample during surgery to remove the brain tumor.
If surgery isn't possible, a sample might be removed with a needle. Removing a sample of brain tumor tissue with a needle is done with a procedure called stereotactic needle biopsy.
During this procedure, a small hole is drilled in the skull. A thin needle is inserted through the hole. The needle is used to take a tissue sample. Imaging tests such as CT and MRI are used to plan the path of the needle. You won't feel anything during the biopsy because medicine is used to numb the area. Often you also receive medicine that puts you in a sleep-like state so you're not aware.
You might have a needle biopsy rather than surgery if your health care team is worried that an operation might hurt an important part of your brain. A needle might be needed to remove tissue from a brain tumor if the tumor is in a spot that's hard to reach with surgery.
Brain biopsy has a risk of complications. Risks include bleeding in the brain and damage to the brain tissue.
- Testing the tissue sample in the lab. The biopsy sample is sent to a lab for testing. Tests can see whether the cells are cancerous or not cancerous. The way the cells look under a microscope can tell your health care team how quickly the cells are growing. This is called the brain tumor's grade. Other tests can find out what DNA changes are present in the cells. This helps your health care team create your treatment plan.
Brain tumor grade
A brain tumor's grade is assigned when the tumor cells are tested in a lab. The grade tells your health care team how quickly the cells are growing and multiplying. The grade is based on how the cells look under a microscope. The grades range from 1 to 4.
A grade 1 brain tumor grows slowly. The cells aren't very different from the healthy cells nearby. As the grade gets higher, the cells undergo changes so that they start to look very different. A grade 4 brain tumor grows very fast. The cells don't look anything like nearby healthy cells.
There are no stages for brain tumors. Other types of cancer have stages. For these other types of cancer, the stage describes how advanced the cancer is and whether it has spread. Brain tumors and brain cancers aren't likely to spread, so they don't have stages.
Prognosis
Your health care team uses all the information from your diagnostic tests to understand your prognosis. The prognosis is how likely it is that the brain tumor can be cured. Things that can influence the prognosis for people with brain tumors include:
- The type of brain tumor.
- How quickly the brain tumor is growing.
- Where the brain tumor is within the brain.
- Which DNA changes are present in the brain tumor cells.
- Whether the brain tumor can be removed completely with surgery.
- Your overall health and well-being.
If you'd like to know more about your prognosis, discuss it with your health care team.
More Information
Treatment
Treatment for a brain tumor depends on whether the tumor is a brain cancer or if it's not cancerous, also called a benign brain tumor. Treatment options also depend on the type, size, grade and location of the brain tumor. Options might include surgery, radiation therapy, radiosurgery, chemotherapy and targeted therapy. When considering your treatment options, your health care team also considers your overall health and your preferences.
Treatment might not be needed right away. You might not need treatment right away if your brain tumor is small, isn't cancerous and doesn't cause symptoms. Small, benign brain tumors might not grow or might grow so slowly that they won't ever cause problems. You might have brain MRI scans a few times a year to check for brain tumor growth. If the brain tumor grows more quickly than expected or if you develop symptoms, you might need treatment.
Surgery
Endoscopic transnasal transsphenoidal surgery

Endoscopic transnasal transsphenoidal surgery
In transnasal transsphenoidal endoscopic surgery, a surgical instrument is placed through the nostril and alongside the nasal septum to access a pituitary tumor.
The goal of surgery for a brain tumor is to remove all of the tumor cells. The tumor can't always be removed completely. When it's possible, the surgeon works to remove as much of the brain tumor as can be done safely. Brain tumor removal surgery can be used to treat brain cancers and benign brain tumors.
Some brain tumors are small and easy to separate from surrounding brain tissue. This makes it likely that the tumor will be removed completely. Other brain tumors can't be separated from surrounding tissue. Sometimes a brain tumor is near an important part of the brain. Surgery might be risky in this situation. The surgeon might take out as much of the tumor as is safe. Removing only part of a brain tumor is sometimes called a subtotal resection.
Removal of part of your brain tumor may help reduce your symptoms.
There are many ways of doing a brain tumor removal surgery. Which option is best for you depends on your situation. Examples of types of brain tumor surgery include:
-
Removing part of the skull to get to the brain tumor. Brain surgery that involves removing part of the skull is called craniotomy. It's the way most brain tumor removal operations are done. Craniotomy is used for treating cancerous brain tumors and benign brain tumors.
The surgeon makes a cut in your scalp. The skin and muscles are moved out of the way. Then the surgeon uses a drill to cut out a section of skull bone. The bone is removed to get access to the brain. If the tumor is deep within the brain, a tool might be used to gently hold healthy brain tissue out of the way. The brain tumor is cut out with special tools. Sometimes lasers are used to destroy the tumor.
During the surgery, you receive medicine to numb the area so you won't feel anything. You're also given medicine that puts you in a sleep-like state during surgery. Sometimes you are awakened during brain surgery. This is called awake brain surgery. When you're awakened, the surgeon might ask questions and monitor the activity in your brain as you respond. This helps lower the risk of hurting important parts of the brain.
When the tumor removal surgery is finished, the part of the skull bone is put back in place.
-
Using a long, thin tube to get to the brain tumor. Endoscopic brain surgery involves putting a long, thin tube into the brain. The tube is called an endoscope. The tube has a series of lenses or a tiny camera that transmits pictures to the surgeon. Special tools are put through the tube to remove the tumor.
Endoscopic brain surgery is often used to treat pituitary tumors. These tumors grow just behind the nasal cavity. The long, thin tube is put through the nose and sinuses and into the brain.
Sometimes endoscopic brain surgery is used to remove brain tumors in other parts of the brain. The surgeon might use a drill to make a hole in the skull. The long, thin tube is carefully put through the brain tissue. The tube continues until it reaches the brain tumor.
Surgery to remove a brain tumor has a risk of side effects and complications. These can include infection, bleeding, blood clots and injury to the brain tissue. Other risks may depend on the part of the brain where the tumor is located. For instance, surgery on a tumor near nerves that connect to the eyes might have a risk of vision loss. Surgery to remove a tumor on a nerve that controls hearing could cause hearing loss.
Radiation therapy
Radiation therapy for brain tumors uses powerful energy beams to kill tumor cells. The energy can come from X-rays, protons and other sources. Radiation therapy for brain tumors usually comes from a machine outside the body. This is called external beam radiation. Rarely, the radiation can be placed inside the body. This is called brachytherapy.
Radiation therapy can be used to treat brain cancers and benign brain tumors.
External beam radiation therapy is usually done in short daily treatments. A typical treatment plan might involve having radiation treatments five days a week for 2 to 6 weeks.
External beam radiation can focus just on the area of your brain where the tumor is located, or it can be applied to your entire brain. Most people with a brain tumor will have radiation aimed at the area around the tumor. If there are many tumors, the entire brain might need radiation treatment. When all of the brain is treated, it's called whole-brain radiation. Whole-brain radiation is most often used to treat cancer that spreads to the brain from another part of the body and forms multiple tumors in the brain.
Traditionally, radiation therapy uses X-rays, but a newer form of this treatment uses energy from protons. The proton beams can be more carefully targeted to only hurt the tumor cells. They may be less likely to hurt nearby healthy tissue. Proton therapy may be helpful for treating brain tumors in children. It also may help in treating tumors that are very close to important parts of the brain. Proton therapy isn't as widely available as traditional X-ray radiation therapy.
Side effects of radiation therapy for brain tumors depend on the type and dose of radiation you receive. Common side effects that happen during treatment or right after it are fatigue, headaches, memory loss, scalp irritation and hair loss. Sometimes radiation therapy side effects show up many years later. These late side effects might include memory and thinking problems.
Radiosurgery
Gamma Knife stereotactic radiosurgery
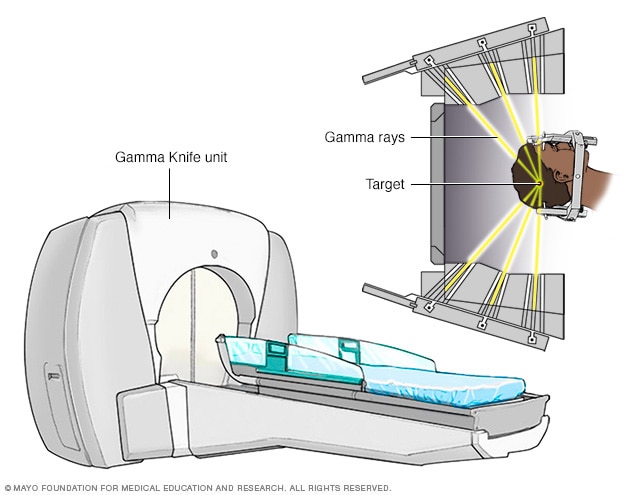
Gamma Knife stereotactic radiosurgery
Stereotactic radiosurgery technology uses many small gamma rays to deliver a precise dose of radiation to the target.
Stereotactic radiosurgery for brain tumors is an intense form of radiation treatment. It aims beams of radiation from many angles at the brain tumor. Each beam isn't very powerful. But the point where the beams meet gets a very large dose of radiation that kills the tumor cells.
Radiosurgery can be used to treat brain cancers and benign brain tumors.
There are different types of technology used in radiosurgery to deliver radiation to treat brain tumors. Some examples include:
- Linear accelerator radiosurgery. Linear accelerator machines also are called LINAC machines. LINAC machines are known by their brand names, such as CyberKnife, TrueBeam and others. A LINAC machine aims carefully shaped beams of energy one at a time from several different angles. The beams are made of X-rays.
- Gamma Knife radiosurgery. A Gamma Knife machine aims many small beams of radiation at the same time. The beams are made of gamma rays.
- Proton radiosurgery. Proton radiosurgery uses beams made of protons. This is the newest type of radiosurgery. It's becoming more common but isn't available at all hospitals.
Radiosurgery is typically done in one treatment or a few treatments. You can go home after treatment and don't need to stay in a hospital.
Side effects of radiosurgery include feeling very tired and skin changes on your scalp. The skin on your head may feel dry, itchy and sensitive. You might have blisters on the skin or hair loss. Sometimes the hair loss is permanent.
Chemotherapy
Chemotherapy for brain tumors uses strong medicines to kill tumor cells. Chemotherapy medicines can be taken in pill form or injected into a vein. Sometimes the chemotherapy medicine is placed in the brain tissue during surgery.
Chemotherapy can be used to treat brain cancers and benign brain tumors. Sometimes it's done at the same time as radiation therapy.
Chemotherapy side effects depend on the type and dose of drugs you receive. Chemotherapy can cause nausea, vomiting and hair loss.
Targeted therapy
Targeted therapy for brain tumors uses medicines that attack specific chemicals present within the tumor cells. By blocking these chemicals, targeted treatments can cause tumor cells to die.
Targeted therapy medicines are available for certain types of brain cancers and benign brain tumors. Your brain tumor cells may be tested to see whether targeted therapy is likely to help you.
Recovering after treatment
After treatment, you might need help to regain function in the part of your brain that had the tumor. You could need help with moving, speaking, seeing and thinking. Based on your specific needs, your health care provider might suggest:
- Physical therapy to help you regain lost motor skills or muscle strength.
- Occupational therapy to help you get back to your typical daily activities, including work.
- Speech therapy to help if speaking is difficult.
- Tutoring for school-age children to help them cope with changes in their memory and thinking.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Alternative medicine
Little research has been done on complementary and alternative brain tumor treatments. No alternative treatments have been proved to cure brain tumors. However, complementary treatments may help you cope with the stress of a brain tumor diagnosis.
Some complementary treatments that may help you cope include:
- Art therapy.
- Exercise.
- Meditation.
- Music therapy.
- Relaxation exercises.
Talk with your health care team about your options.
Coping and support
Some people say a brain tumor diagnosis feels overwhelming and frightening. It might make you feel like you have little control over your health. It might help to take steps to understand your condition and talk about your feelings. Consider trying to:
- Learn enough about brain tumors to make decisions about your care. Ask your health care provider about your specific type of brain tumor. Ask about your treatment options and, if you like, your prognosis. As you learn more about brain tumors, you may feel better about making treatment decisions. Seek out information from reliable sources, such as the American Cancer Society and the National Cancer Institute.
- Keep friends and family close. Keeping your close relationships strong will help you deal with your brain tumor. Friends and family can provide the practical support you'll need, such as helping take care of your home if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by cancer.
Find someone to talk with. Find a good listener who is willing to hear you talk about your hopes and fears. This may be a friend, family member or clergy member. Ask your health care team to suggest a counselor or medical social worker you can talk with.
Ask your health care team about brain tumor support groups in your area. It can be helpful to learn how others in your same situation are coping with complicated medical problems.
Preparing for your appointment
Make an appointment with your usual health care provider if you have any symptoms that worry you. If you're diagnosed with a brain tumor, you may be referred to specialists. These might include:
- Doctors who specialize in brain disorders, called neurologists.
- Doctors who use medicine to treat cancer, called medical oncologists.
- Doctors who use radiation to treat cancer, called radiation oncologists.
- Doctors who specialize in nervous system cancers, called neuro-oncologists.
- Surgeons who operate on the brain and nervous system, called neurosurgeons.
- Rehabilitation specialists.
- Providers who specialize in helping with memory and thinking problems that can happen in people with brain tumors. These providers are called psychologists or behavioral psychologists.
It's a good idea to be prepared for your appointment. Here's some information to help you get ready.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you're taking.
- Consider taking a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who goes with you may remember something that you missed or forgot. That person can help you understand what your health care team is telling you.
- Write down questions to ask your doctor.
Your time with your health care provider is limited. Prepare a list of questions to help you make the most of your time together. Identify the three questions that are most important to you. List the rest of the questions from most important to least important in case time runs out. For a brain tumor, some basic questions to ask include:
- What type of brain tumor do I have?
- Where is my brain tumor located?
- How large is my brain tumor?
- How aggressive is my brain tumor?
- Is my brain tumor cancerous?
- Will I need additional tests?
- What are my treatment options?
- Can any treatments cure my brain tumor?
- What are the benefits and risks of each treatment?
- Is there one treatment you think is best for me?
- What happens if the first treatment doesn't work?
- What happens if I choose to not have treatment?
- I know that you can't predict the future, but am I likely to survive my brain tumor? What can you tell me about the survival rate of people with this diagnosis?
- Should I see a specialist? What will that cost, and will my insurance cover it?
- Should I seek care at a medical center or hospital that has experience in treating brain tumors?
- Are there brochures or other printed material that I can take with me? What websites do you recommend?
- What will determine whether I should plan for a follow-up visit?
In addition to the questions that you've prepared, don't hesitate to ask other questions that occur to you.
What to expect from your doctor
Your provider is likely to ask you a number of questions. Being ready to answer them may allow time later to cover other points you want to address. Your doctor may ask:
- When did you first begin experiencing symptoms?
- Do your symptoms happen all the time or do they come and go?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?