Diagnosis
Bladder cancer FAQs
Get answers to the most frequently asked questions about bladder cancer from urologist Mark Tyson, M.D., M.P.H.
Hi. I'm Dr. Mark Tyson, a urologist at Mayo Clinic, and I'm here to answer some of the important questions you might have about bladder cancer.
What type of bladder cancer do I have?
The type of bladder cancer that most patients are diagnosed with is urothelial carcinoma. There are other types of cancers of the bladder, like adenocarcinomas and small cell carcinomas, but urothelial carcinoma is the most common. Some urothelial carcinomas have what's called variant histology, and these can be plasmacytoid, micropapillary, microcystic. These are tumors that generally increase the aggressiveness of the urothelial carcinoma. But in addition to the cell type, you'd also need to know the grade and the stage of your tumor. These tumors are generally graded as low grade and high grade, with high-grade cancers being more aggressive. The grade, the stage, and the type of cancer are all used to determine the type of treatment that you will receive.
What are my treatment options?
The treatment options depend on the grade and stage of your tumor. If you have a high-grade, non-muscle-invasive bladder cancer, we generally treat that with a transurethral resection of the bladder tumor, followed by intravesicle therapy, either with chemotherapy or immunotherapy, like BCG. If you have an invasive carcinoma, such as a muscle-invasive cancer, we generally treat that with upfront cisplatin-based combination chemotherapy, followed by removal of the bladder or radiation. There are quality of life and toxicity considerations with each of those options, and it's up to the individual to decide which is right for them. Adjuvant immunotherapy is a type of treatment that's given after surgery to help mitigate the risk of cancer recurrence down the road. Patients who have stage 4 bladder cancer are generally treated with first-line cisplatin-based combination chemotherapy.
Should I have my surgery done robotically?
The short answer is it really doesn't matter. Whether you had the surgery done open or whether you have it done robotically, the outcomes are about the same. This is a big operation and patients are going to be in the hospital for a few days after surgery and require a few weeks to recover, no matter how the surgery is done. With a robotic approach, though, there are tiny laparoscopic incisions. And in general, there's a little bit less blood loss and perhaps a few fewer wound complications. With the open approach, the surgery is faster, but associated with a little bit more blood loss. And I encourage patients to go with the surgery that feels right for themselves.
What is a neobladder?
A neobladder is a type of urinary diversion that's performed during the surgery to remove the bladder. So, when we remove the bladder, we have to reroute the urine somewhere. And what we do is we take about a foot of small intestines, called ileum, and we detubularize it, or fillet it, open. We create it into a sphere. And then we connect that down to the urethra and then we connect the kidneys into that. And it's nice because all of the hardware, so to speak, is on the inside of the body. There's no external drainage bag for urine, like there is with an ileal conduit. But there are some downsides to a neobladder. They don't work perfectly. For example, about 25% of men will have some degree of long-term incontinence, and about 30% of women. About 10% of men will need to catheterize to empty their neobladder and about 25% of women will, as well. And these are important considerations as one is deciding between a neobladder and a conduit.
What is an ileal conduit?
An ileal conduit is a form of urinary diversion where there's an external bag used for drainage. Unlike a neobladder where we build a new bladder and connect the kidneys to the urethra and everything's on the inside of the body, an ileal conduit diverts the urine outside of the body. So just to the right of your belly button there'll be a stoma, like an ostomy, that drains into a bag. For lots of patients, this is the best option. It's simple and it's easy to learn how to use. There's no getting up at night to use the restroom. There's no stopping when you're driving. And anything that you were doing before surgery, you can do after. This includes scuba diving, skydiving, water skiing, golfing, hiking, biking. Lots of patients ask the question of what's the right diversion for me? And it just really depends upon the individual. For individuals who are looking for simplicity, the ileal conduit is the right choice.
How will treatment affect my quality of life?
Quality of life is a very important consideration when deciding what treatment options are best for you. For non-muscle-invasive bladder cancer, we generally treat with intravesicle therapy. But there are side effects of treatment: Burning pain with urination, frequency, urgency, blood in the urine. They also involve catheterizations and can be painful during administrations. For patients who have muscle-invasive disease, and they're trying to decide between whether to do a cystectomy, which is complete removal of the bladder, or radiation therapy, there are a number of quality of life implications there as well.
How can I be the best partner to my medical team?
Patients who are invested in their care are the easiest to take care of. Learn as much as you can. And remember, we're all on the same team. Never hesitate to ask your medical team any questions or concerns you have. Being informed makes all the difference. Thanks for your time and we wish you well.
Diagnosing bladder cancer
Female cystoscopy
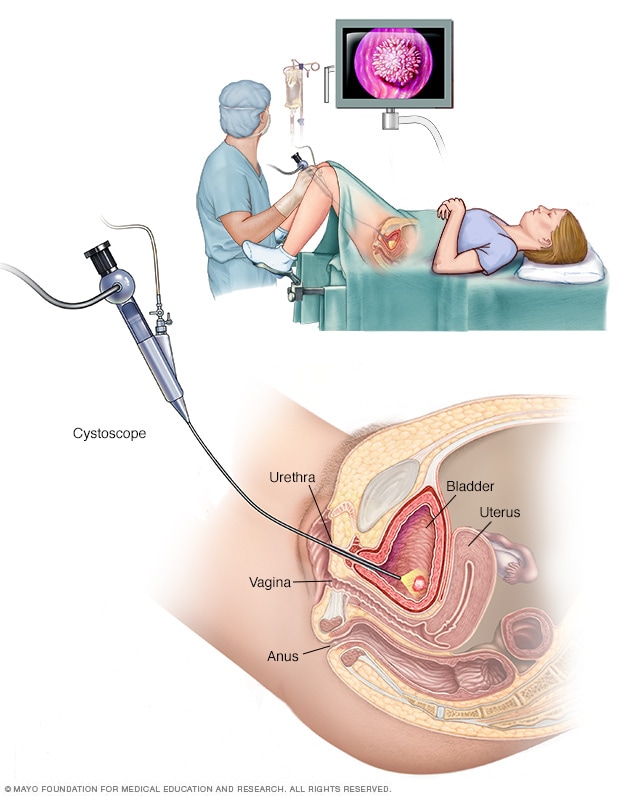
Female cystoscopy
Cystoscopy allows a health care provider to view the lower urinary tract to look for problems, such as a bladder stone. Surgical tools can be passed through the cystoscope to treat certain urinary tract conditions.
Male cystoscopy
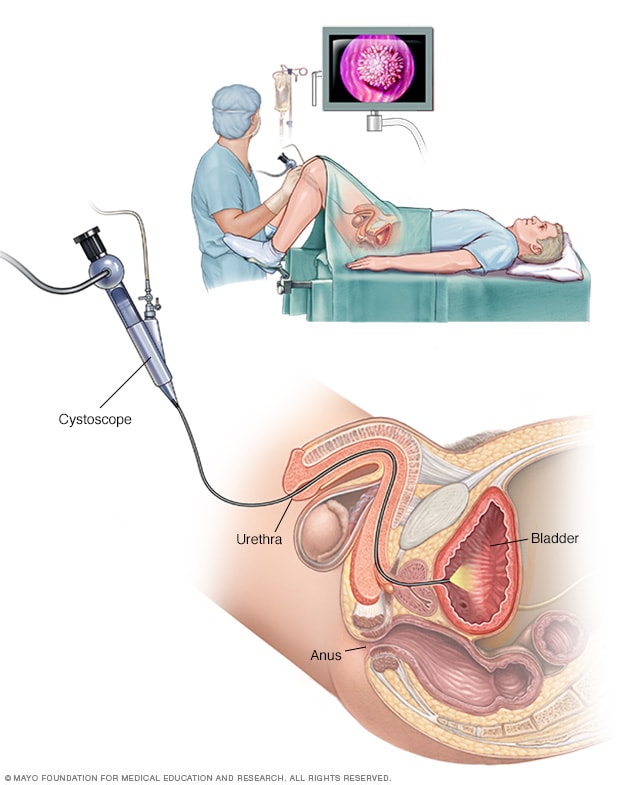
Male cystoscopy
Cystoscopy allows a health care provider to view the lower urinary tract to look for problems in the urethra and bladder. Surgical tools can be passed through the cystoscope to treat certain urinary tract conditions.
Tests and procedures used to diagnose bladder cancer may include:
- Using a scope to examine the inside of your bladder (cystoscopy). To perform cystoscopy, your doctor inserts a small, narrow tube (cystoscope) through your urethra. The cystoscope has a lens that allows your doctor to see the inside of your urethra and bladder, to examine these structures for signs of disease. Cystoscopy can be done in a doctor's office or in the hospital.
- Removing a sample of tissue for testing (biopsy). During cystoscopy, your doctor may pass a special tool through the scope and into your bladder to collect a cell sample (biopsy) for testing. This procedure is sometimes called transurethral resection of bladder tumor (TURBT). TURBT can also be used to treat bladder cancer.
- Examining a urine sample (urine cytology). A sample of your urine is analyzed under a microscope to check for cancer cells in a procedure called urine cytology.
-
Imaging tests. Imaging tests, such as computerized tomography (CT) urogram or retrograde pyelogram, allow your doctor to examine the structures of your urinary tract.
During a CT urogram, a contrast dye injected into a vein in your hand eventually flows into your kidneys, ureters and bladder. X-ray images taken during the test provide a detailed view of your urinary tract and help your doctor identify any areas that might be cancer.
Retrograde pyelogram is an X-ray exam used to get a detailed look at the upper urinary tract. During this test, your doctor threads a thin tube (catheter) through your urethra and into your bladder to inject contrast dye into your ureters. The dye then flows into your kidneys while X-ray images are captured.
Determining the extent of the cancer
After confirming that you have bladder cancer, your doctor may recommend additional tests to determine whether your cancer has spread to your lymph nodes or to other areas of your body.
Tests may include:
- CT scan
- Magnetic resonance imaging (MRI)
- Positron emission tomography (PET)
- Bone scan
- Chest X-ray
Your doctor uses information from these procedures to assign your cancer a stage. The stages of bladder cancer are indicated by Roman numerals ranging from 0 to IV. The lowest stages indicate a cancer that's confined to the inner layers of the bladder and that hasn't grown to affect the muscular bladder wall. The highest stage — stage IV — indicates cancer that has spread to lymph nodes or organs in distant areas of the body
Bladder cancer grade
Bladder cancers are further classified based on how the cancer cells appear when viewed through a microscope. This is known as the grade, and your doctor may describe bladder cancer as either low grade or high grade:
- Low-grade bladder cancer. This type of cancer has cells that are closer in appearance and organization to normal cells (well differentiated). A low-grade tumor usually grows more slowly and is less likely to invade the muscular wall of the bladder than is a high-grade tumor.
- High-grade bladder cancer. This type of cancer has cells that are abnormal-looking and that lack any resemblance to normal-appearing tissues (poorly differentiated). A high-grade tumor tends to grow more aggressively than a low-grade tumor and may be more likely to spread to the muscular wall of the bladder and other tissues and organs.
More Information
Treatment
Treatment options for bladder cancer depend on a number of factors, including the type of cancer, grade of the cancer and stage of the cancer, which are taken into consideration along with your overall health and your treatment preferences.
Bladder cancer treatment may include:
- Surgery, to remove the cancer cells
- Chemotherapy in the bladder (intravesical chemotherapy), to treat cancers that are confined to the lining of the bladder but have a high risk of recurrence or progression to a higher stage
- Chemotherapy for the whole body (systemic chemotherapy), to increase the chance for a cure in a person having surgery to remove the bladder, or as a primary treatment when surgery isn't an option
- Radiation therapy, to destroy cancer cells, often as a primary treatment when surgery isn't an option or isn't desired
- Immunotherapy, to trigger the body's immune system to fight cancer cells, either in the bladder or throughout the body
- Targeted therapy, to treat advanced cancer when other treatments haven't helped
A combination of treatment approaches may be recommended by your doctor and members of your care team.
Bladder cancer surgery
Ileal conduit

Ileal conduit
During an ileal conduit procedure, a surgeon makes a new tube from a piece of intestine that allows the kidneys to drain and urine to exit the body through a small opening called a stoma.
Neobladder reconstruction

Neobladder reconstruction
During neobladder surgery, a surgeon takes out the existing bladder and forms a pouch inside the body from part of the intestine. The pouch, called a neobladder, stores urine.
Approaches to bladder cancer surgery might include:
-
Transurethral resection of bladder tumor (TURBT). TURBT is a procedure to diagnose bladder cancer and to remove cancers confined to the inner layers of the bladder — those that aren't yet muscle-invasive cancers. During the procedure, a surgeon passes an electric wire loop through a cystoscope and into the bladder. The electric current in the wire is used to cut away or burn away the cancer. Alternatively, a high-energy laser may be used.
Because doctors perform the procedure through the urethra, you won't have any cuts (incisions) in your abdomen.
As part of the TURBT procedure, your doctor may recommend a one-time injection of cancer-killing medication (chemotherapy) into your bladder to destroy any remaining cancer cells and to prevent cancer from coming back. The medication remains in your bladder for a period of time and then is drained.
-
Cystectomy. Cystectomy is surgery to remove all or part of the bladder. During a partial cystectomy, your surgeon removes only the portion of the bladder that contains a single cancerous tumor.
A radical cystectomy is an operation to remove the entire bladder and the surrounding lymph nodes. In men, radical cystectomy typically includes removal of the prostate and seminal vesicles. In women, radical cystectomy may involve removal of the uterus, ovaries and part of the vagina.
Radical cystectomy can be performed through an incision on the lower portion of the belly or with multiple small incisions using robotic surgery. During robotic surgery, the surgeon sits at a nearby console and uses hand controls to precisely move robotic surgical instruments.
- Neobladder reconstruction. After a radical cystectomy, your surgeon must create a new way for urine to leave your body (urinary diversion). One option for urinary diversion is neobladder reconstruction. Your surgeon creates a sphere-shaped reservoir out of a piece of your intestine. This reservoir, often called a neobladder, sits inside your body and is attached to your urethra. The neobladder allows most people to urinate normally. A small number of people difficulty emptying the neobladder and may need to use a catheter periodically to drain all the urine from the neobladder.
- Ileal conduit. For this type of urinary diversion, your surgeon creates a tube (ileal conduit) using a piece of your intestine. The tube runs from your ureters, which drain your kidneys, to the outside of your body, where urine empties into a pouch (urostomy bag) you wear on your abdomen.
- Continent urinary reservoir. During this type of urinary diversion procedure, your surgeon uses a section of intestine to create a small pouch (reservoir) to hold urine, located inside your body. You drain urine from the reservoir through an opening in your abdomen using a catheter a few times each day.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. Chemotherapy treatment for bladder cancer usually involves two or more chemotherapy drugs used in combination.
Chemotherapy drugs can be given:
- Through a vein (intravenously). Intravenous chemotherapy is frequently used before bladder removal surgery to increase the chances of curing the cancer. Chemotherapy may also be used to kill cancer cells that might remain after surgery. In certain situations, chemotherapy may be combined with radiation therapy.
- Directly into the bladder (intravesical therapy). During intravesical chemotherapy, a tube is passed through your urethra directly to your bladder. The chemotherapy is placed in the bladder for a set period of time before being drained. It can be used as the primary treatment for superficial bladder cancer, where the cancer cells affect only the lining of the bladder and not the deeper muscle tissue.
Radiation therapy
Radiation therapy uses beams of powerful energy, such as X-rays and protons, to destroy the cancer cells. Radiation therapy for bladder cancer usually is delivered from a machine that moves around your body, directing the energy beams to precise points.
Radiation therapy is sometimes combined with chemotherapy to treat bladder cancer in certain situations, such as when surgery isn't an option or isn't desired.
Immunotherapy
Immunotherapy is a drug treatment that helps your immune system to fight cancer.
Immunotherapy can be given:
- Directly into the bladder (intravesical therapy). Intravesical immunotherapy might be recommended after TURBT for small bladder cancers that haven't grown into the deeper muscle layers of the bladder. This treatment uses bacillus Calmette-Guerin (BCG), which was developed as a vaccine used to protect against tuberculosis. BCG causes an immune system reaction that directs germ-fighting cells to the bladder.
- Through a vein (intravenously). Immunotherapy can be given intravenously for bladder cancer that's advanced or that comes back after initial treatment. Several immunotherapy drugs are available. These drugs help your immune system identify and fight the cancer cells.
Targeted therapy
Targeted therapy drugs focus on specific weaknesses present within cancer cells. By targeting these weaknesses, targeted drug treatments can cause cancer cells to die. Your cancer cells may be tested to see if targeted therapy is likely to be effective.
Targeted therapy may be an option for treating advanced bladder cancer when other treatments haven't helped.
Bladder preservation
In certain situations, people with muscle-invasive bladder cancer who don't want to undergo surgery to remove the bladder may consider trying a combination of treatments instead. Known as trimodality therapy, this approach combines TURBT, chemotherapy and radiation therapy.
First, your surgeon performs a TURBT procedure to remove as much of the cancer as possible from your bladder while preserving bladder function. After TURBT, you undergo a regimen of chemotherapy along with radiation therapy.
If, after trying trimodality therapy, not all of the cancer is gone or you have a recurrence of muscle-invasive cancer, your doctor may recommend a radical cystectomy.
After bladder cancer treatment
Bladder cancer may recur, even after successful treatment. Because of this, people with bladder cancer need follow-up testing for years after successful treatment. What tests you'll have and how often depends on your type of bladder cancer and how it was treated, among other factors.
In general, doctors recommend a test to examine the inside of your urethra and bladder (cystoscopy) every three to six months for the first few years after bladder cancer treatment. After a few years of surveillance without detecting cancer recurrence, you may need a cystoscopy exam only once a year. Your doctor may recommend other tests at regular intervals as well.
People with aggressive cancers may undergo more-frequent testing. Those with less aggressive cancers may undergo testing less often.
Related video
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
Living with the concern that your bladder cancer may recur can leave you feeling as if you have little control over your future. But while there's no way to ensure that your bladder cancer won't recur, you can take steps to manage the stress.
Over time you'll find what works for you, but until then, you might:
- Get a schedule of follow-up tests and go to each appointment. When you finish bladder cancer treatment, ask your doctor to create a personalized schedule of follow-up tests. Before each follow-up cystoscopy exam, expect to have some anxiety. You may fear that cancer has come back or worry about the uncomfortable exam. But don't let this stop you from going to your appointment. Instead, plan ways to cope with your concerns. Write your thoughts in a journal, talk with a friend or use relaxation techniques, such as meditation.
- Take care of yourself so that you're ready to fight cancer if it comes back. Take care of yourself by adjusting your diet to include plenty of fruits, vegetables and whole grains. Exercise for at least 30 minutes most days of the week. Get enough sleep so that you wake feeling rested.
- Talk with other bladder cancer survivors. Connect with bladder cancer survivors who are experiencing the same fears you're feeling. Contact your local chapter of the American Cancer Society to ask about support groups in your area.
Preparing for your appointment
Start by seeing your family doctor if you have any signs or symptoms that worry you, such as blood in your urine. Your doctor may suggest tests and procedures to investigate your signs and symptoms.
If your doctor suspects that you may have bladder cancer, you may be referred to a doctor who specializes in treating diseases and conditions of the urinary tract (urologist). In some cases, you may be referred to other specialists, such as doctors who treat cancer (oncologists).
Because there's often a lot of information to discuss, it's a good idea to be well prepared. Here's some information to help you get ready, and what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you're experiencing, including any that seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements that you're taking along with dosages.
- Consider taking a family member or friend along. Sometimes it's difficult to remember all of the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your doctor.
Preparing a list of questions can help you make the most of your time with your doctor. For bladder cancer, some basic questions to ask include:
- Do I have bladder cancer or could my symptoms be caused by another condition?
- What is the stage of my cancer?
- Will I need any additional tests?
- What are my treatment options?
- Can any treatments cure my bladder cancer?
- What are the potential risks of each treatment?
- Is there one treatment that you feel is best for me?
- Should I see a specialist? What will that cost, and will my insurance cover it?
- Is there a generic alternative to the medicine you're prescribing me?
- Are there brochures or other printed material that I can take with me? What websites do you recommend?
- What will determine whether I should plan for a follow-up visit?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask other questions that occur to you.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may allow time later to cover other points you want to address. Your doctor may ask:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?