Overview
Amenorrhea (uh-men-o-REE-uh) is the absence of menstruation, often defined as missing one or more menstrual periods.
Primary amenorrhea refers to the absence of menstruation in someone who has not had a period by age 15. The most common causes of primary amenorrhea relate to hormone levels, although anatomical problems also can cause amenorrhea.
Secondary amenorrhea refers to the absence of three or more periods in a row by someone who has had periods in the past. Pregnancy is the most common cause of secondary amenorrhea, although problems with hormones also can cause secondary amenorrhea.
Treatment of amenorrhea depends on the underlying cause.
Products & Services
Symptoms
Depending on the cause of amenorrhea, you might experience other signs or symptoms along with the absence of periods, such as:
- Milky nipple discharge
- Hair loss
- Headache
- Vision changes
- Excess facial hair
- Pelvic pain
- Acne
When to see a doctor
Consult your doctor if you've missed at least three menstrual periods in a row, or if you've never had a menstrual period and you're age 15 or older.
Causes
Female reproductive system
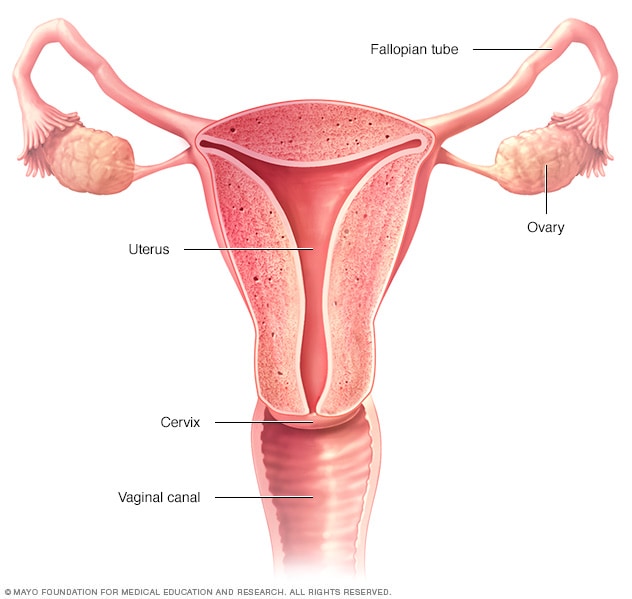
Female reproductive system
The ovaries, fallopian tubes, uterus, cervix and vagina, also called the vaginal canal, make up the female reproductive system.
Amenorrhea can occur for a variety of reasons. Some are normal, while others may be a side effect of medication or a sign of a medical problem.
Natural amenorrhea
During the normal course of your life, you may experience amenorrhea for natural reasons, such as:
- Pregnancy
- Breastfeeding
- Menopause
Contraceptives
Some people who take birth control pills (oral contraceptives) may not have periods. Even after stopping birth control pills, it may take some time before regular ovulation and menstruation return. Contraceptives that are injected or implanted also may cause amenorrhea, as can some types of intrauterine devices.
Medications
Certain medications can cause menstrual periods to stop, including some types of:
- Antipsychotics
- Cancer chemotherapy
- Antidepressants
- Blood pressure drugs
- Allergy medications
Lifestyle factors
Sometimes lifestyle factors contribute to amenorrhea, for instance:
- Low body weight. Excessively low body weight — about 10% under normal weight — interrupts many hormonal functions in the body, potentially halting ovulation. Women who have an eating disorder, such as anorexia or bulimia, often stop having periods because of these abnormal hormonal changes.
- Excessive exercise. Women who participate in activities that require rigorous training, such as ballet, may find their menstrual cycles interrupted. Several factors combine to contribute to the loss of periods in athletes, including low body fat, stress and high energy expenditure.
- Stress. Mental stress can temporarily alter the functioning of your hypothalamus — an area of your brain that controls the hormones that regulate your menstrual cycle. Ovulation and menstruation may stop as a result. Regular menstrual periods usually resume after your stress decreases.
Hormonal imbalance
Many types of medical problems can cause hormonal imbalance, including:
- Polycystic ovary syndrome (PCOS). PCOS causes relatively high and sustained levels of hormones, rather than the fluctuating levels seen in the normal menstrual cycle.
- Thyroid malfunction. An overactive thyroid gland (hyperthyroidism) or underactive thyroid gland (hypothyroidism) can cause menstrual irregularities, including amenorrhea.
- Pituitary tumor. A noncancerous (benign) tumor in your pituitary gland can interfere with the hormonal regulation of menstruation.
- Premature menopause. Menopause usually begins around age 50. But, for some women, the ovarian supply of eggs diminishes before age 40 and menstruation stops.
Structural problems
Problems with the sexual organs themselves also can cause amenorrhea. Examples include:
- Uterine scarring. Asherman's syndrome, a condition in which scar tissue builds up in the lining of the uterus, can sometimes occur after a dilation and curettage (D&C), cesarean section or treatment for uterine fibroids. Uterine scarring prevents the normal buildup and shedding of the uterine lining.
- Lack of reproductive organs. Sometimes problems arise during fetal development that lead to missing parts of the reproductive system, such as the uterus, cervix or vagina. Because the reproductive system didn't develop fully, menstrual cycles aren't possible later in life.
- Structural abnormality of the vagina. An obstruction of the vagina may prevent visible menstrual bleeding. A membrane or wall may be present in the vagina that blocks the outflow of blood from the uterus and cervix.
Ovulation is the release of an egg from one of the ovaries. It often happens about midway through the menstrual cycle, although the exact timing may vary.
In preparation for ovulation, the lining of the uterus, or endometrium, thickens. The pituitary gland in the brain stimulates one of the ovaries to release an egg. The wall of the ovarian follicle ruptures at the surface of the ovary. The egg is released.
Finger-like structures called fimbriae sweep the egg into the neighboring fallopian tube. The egg travels through the fallopian tube, propelled in part by contractions in the fallopian tube walls. Here in the fallopian tube, the egg may be fertilized by a sperm.
If the egg is fertilized, the egg and sperm unite to form a one-celled entity called a zygote. As the zygote travels down the fallopian tube toward the uterus, it begins dividing rapidly to form a cluster of cells called a blastocyst, which resembles a tiny raspberry. When the blastocyst reaches the uterus, it implants in the lining of the uterus and pregnancy begins.
If the egg isn't fertilized, it's simply reabsorbed by the body — perhaps before it even reaches the uterus. About two weeks later, the lining of the uterus sheds through the vagina. This is known as menstruation.
Risk factors
Factors that may increase your risk of amenorrhea include:
- Family history. If other women in your family have experienced amenorrhea, you may have inherited a predisposition for the problem.
- Eating disorders. If you have an eating disorder, such as anorexia or bulimia, you are at higher risk of developing amenorrhea.
- Athletic training. Rigorous athletic training can increase your risk of amenorrhea.
- History of certain gynecologic procedures. If you've had a D&C, especially related to pregnancy, or a procedure known as loop electrodiathermy excision procedure (LEEP), your risk of developing amenorrhea is higher.
Complications
The causes of amenorrhea can cause other problems as well. These include:
- Infertility and problems with pregnancy. If you don't ovulate and don't have menstrual periods, you can't become pregnant. When hormone imbalance is the cause of amenorrhea, this can also cause miscarriage or other problems with pregnancy.
- Psychological stress. Not having periods when your peers are having theirs can be stressful, especially for young people who are transitioning into adulthood.
- Osteoporosis and cardiovascular disease. These two problems can be caused by not having enough estrogen. Osteoporosis is a weakening of the bones. Cardiovascular disease includes heart attack and problems with the blood vessels and heart muscle.
- Pelvic pain. If an anatomical problem is causing the amenorrhea, it may also cause pain in the pelvic area.
Feb. 09, 2023