Overview
The liver
The liver
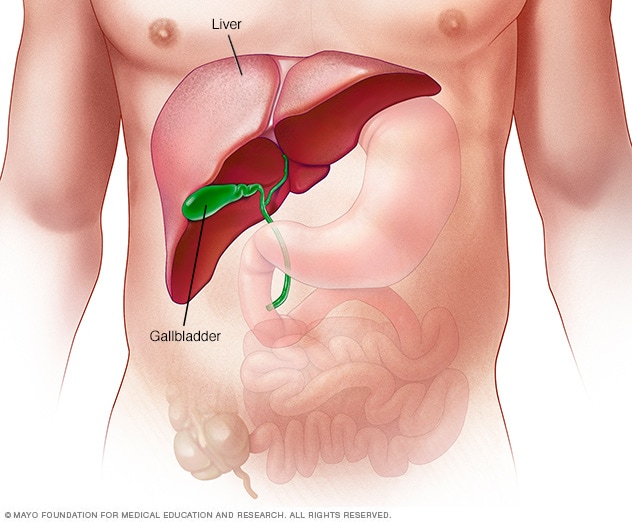
The liver is your largest internal organ. About the size of a football, it's located mainly in the upper right portion of your abdomen, beneath the diaphragm and above your stomach.
Alcoholic hepatitis is swelling, called inflammation, of the liver caused by drinking alcohol. Drinking alcohol destroys liver cells.
Alcoholic hepatitis most often happens in people who drink heavily over many years. But the link between drinking and alcoholic hepatitis isn't simple. Not all heavy drinkers get alcoholic hepatitis. And some people who drink much less get the disease.
If you're diagnosed with alcoholic hepatitis, you must stop drinking alcohol. People who keep drinking alcohol have a high risk of serious liver damage and death.
Products & Services
Symptoms
The most common sign of alcoholic hepatitis is yellowing of the skin and whites of the eyes, called jaundice. The yellowing of the skin might be harder to see on Black and brown people.
Other symptoms include:
- Loss of appetite.
- Nausea and vomiting.
- Belly tenderness.
- Fever, often low grade.
- Tiredness and weakness.
People with alcoholic hepatitis tend to be malnourished. Drinking large amounts of alcohol keeps people from being hungry. And heavy drinkers get most of their calories from alcohol.
Other symptoms that happen with severe alcoholic hepatitis include:
- Fluid buildup in the belly, called ascites.
- Being confused and acting oddly due to a buildup of toxins. The healthy liver breaks these toxins down and gets rid of them.
- Kidney and liver failure.
When to see a doctor
Alcoholic hepatitis is a serious, often deadly disease.
See a healthcare professional if you:
- Have symptoms of alcoholic hepatitis.
- Can't control your drinking.
- Want help cutting back on your drinking.
Causes
Alcoholic hepatitis is caused by damage to the liver from drinking alcohol. Just how alcohol damages the liver and why it does so only in some heavy drinkers isn't clear.
These factors are known to play a role in alcoholic hepatitis:
- The body's way of breaking down alcohol makes highly toxic chemicals.
- These chemicals trigger swelling, called inflammation, that destroys liver cells.
- Over time, scars replace healthy liver tissue. This keeps the liver from working well.
- This scarring, called cirrhosis, can't be fixed. It's the final stage of alcoholic liver disease.
Other factors that can be involved with alcoholic hepatitis include:
- Other types of liver disease. Alcoholic hepatitis can make chronic liver diseases worse. For instance, if you have hepatitis C and drink, even a little, you're more likely to get liver scarring than if you don't drink.
- Lack of nutrition. Many people who drink heavily don't get enough nutrients because they eat poorly. And alcohol keeps the body from using nutrients as it should. Lack of nutrients can damage liver cells.
Risk factors
The major risk factor for alcoholic hepatitis is the how much alcohol you drink. It isn't known how much alcohol it takes to cause alcoholic hepatitis.
Most people with this condition have had at least seven drinks a day for 20 years or more. This can mean 7 glasses of wine, 7 beers, or 7 shots of spirits.
However, alcoholic hepatitis can happen to people who drink less and have other risk factors, including:
- Sex. Women seem to have a higher risk of getting alcoholic hepatitis. That might be because of how alcohol breaks down in women's bodies.
- Obesity. Heavy drinkers who are overweight might be more likely to get alcoholic hepatitis. And they might be more likely to go on to get liver scarring.
- Genes. Studies suggest that genes might be involved in alcohol-induced liver disease.
- Race and ethnicity. Black and Hispanic people might be at higher risk of alcoholic hepatitis.
- Binge drinking. Having five or more drinks in about two hours for men and four or more for women might increase the risk of alcoholic hepatitis.
Complications
Esophageal varices

Esophageal varices
Esophageal varices are enlarged veins in the esophagus. They're often due to blocked blood flow through the portal vein. The portal vein carries blood from the intestine, pancreas and spleen to the liver.
Typical liver vs. liver cirrhosis
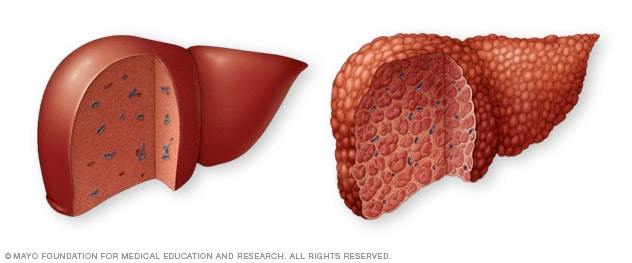
Typical liver vs. liver cirrhosis
A typical liver (left) shows no signs of scarring. In cirrhosis (right), scar tissue replaces healthy liver tissue.
Complications of alcoholic hepatitis are caused by scar tissue on the liver. Scar tissue can slow blood flow through the liver. That can raise pressure in a major blood vessel called the portal vein and cause a buildup of toxins.
Complications include:
-
Enlarged veins, called varices. Blood that can't flow freely through the portal vein can back up into other blood vessels in the stomach and the tube through which food passes from the throat to the stomach, called the esophagus.
These blood vessels have thin walls. They're likely to bleed if filled with too much blood. Heavy bleeding in the upper stomach or esophagus is life-threatening and needs medical care right away.
- Ascites (ah-SITE-ees). Fluid that builds up in the belly might get infected and need treatment with antibiotics. Ascites isn't life-threatening. But it most often means advanced alcoholic hepatitis or cirrhosis.
- Confusion, drowsiness and slurred speech, called hepatic encephalopathy. A damaged liver has trouble removing toxins from the body. The buildup of toxins can damage the brain. Severe hepatic encephalopathy can cause a coma.
- Kidney failure. A damaged liver can affect blood flow to the kidneys. This can damage the kidneys.
- Cirrhosis. This scarring of the liver can lead to liver failure.
Prevention
You might reduce your risk of alcoholic hepatitis if you:
- Drink alcohol in moderation, if at all. For healthy adults, moderate drinking means up to one drink a day for women and up to two drinks a day for men. The only certain way to prevent alcoholic hepatitis is to avoid all alcohol.
- Protect yourself from hepatitis C. Hepatitis C is a liver disease caused by a virus. Without treatment, it can lead to cirrhosis. If you have hepatitis C and drink alcohol, you're far more likely to get cirrhosis than if you don't drink.
-
Check before mixing medicines and alcohol. Ask your healthcare professional if it's safe to drink alcohol when taking your prescribed medicines. Read the warning labels on medicines you can get without a prescription.
Don't drink alcohol when taking medicines that warn against drinking alcohol while taking them. This includes pain relievers such as acetaminophen (Tylenol, others).
Nov. 09, 2023